INTRODUCTION
Imaging recording in the surgical field is important for the education and training of new surgeons. In past decades, independent camcorders were used for recording, separated from the surgeon and another person was needed to record the images. Sometimes, a light-mounted recorder was used but it was expensive, and field of view was be limited by the position and motion of the surgeon. Some surgeons use commercially available digital camcorders and attach it on a handle of a surgical light or a holding arm for camera1,2). A surgical microscope could record images but in the neurotrauma field, a microscope is used less frequently than other neurosurgical fields.
Recently, digital devices have become small enough to attach to a surgeon’s head, and indeed recorded image quality has been improved. Wearable camcorders were introduced in the market for sports and leisure, but their performance and small size has also made them available in medical fields8,9). We used one of these wearable and cheap devices for surgical image recording in traumatic brain injury (TBI), then evaluated its safety and feasibility.
MATERIALS AND METHODS
1. Technical Specifications of the Camcorder
We purchased an HX-A500 action camera (up to 32 GB storage-SDHC card, 2 hr long internal battery, waterproof, Wi-Fi control, 1080 p 60 frames per sec[fps], 2160 p 24 fps; Panasonic, Osaka, Japan), which was cheaper than a professional video recording system.
2. Wearing the Device
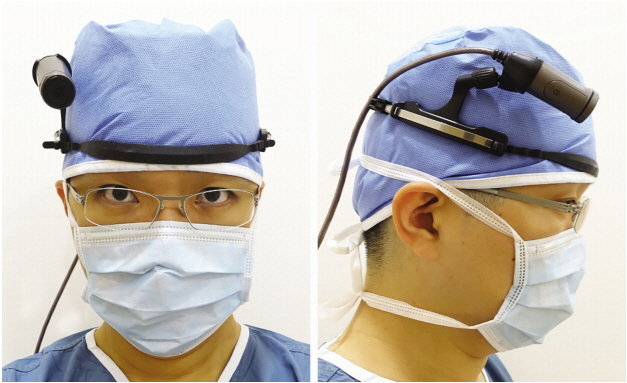
A single surgeon used this camcorder as an operator during TBI surgery. This camera consisted of a small round camera unit and a square-shaped control unit connected to a 70-cm long cable. The head mounting accessory was included and it was attached to the surgeon’s head (Fig. 1). The control unit was attached to an armband on the surgeon’s upper arm. It was controlled by push buttons on a surgical gown or by wireless remote control. The head unit and the arm control unit were worn before surgical scrubbing.
3. Recording and Storage of Video Files
Recording image quality was set to 1080 p 60 fps with normal field of view. Movie files were stored with h264 codec, in 0.19 GB size per min. Starting time was decided by the surgeon and scalp incision and retraction was not routinely recorded due to limited battery life.
Recorded video files were transferred immediately after surgery in a password-locked hard disk drive on a Windows computer system. They were sorted by date and reviewed. Video files were reviewed by a neurosurgeon. We checked the following aspects: the center of the image matched to the surgeon’s view or center of surgical field, image quality, and overexposure or underexposure which can distort the image detail.
4. Review by Residents
Recorded movie clips were shown to the residents of our institute. First-grade residents were not included as reviewers because they had not experienced an operating room. A total of six residents (from 2nd to 4th grade, each grade having two people) participated in reviewing the images and then answered the questions (Table 1) We assessed the understanding of the whole sequence of surgery, sharing of operator’s field of view, education for the main operator, and how to manage an emergency situation. According to the degree of assistance provided by the video recording, 1 to 5 points could be assigned to each of the assigned criteria.
RESULTS
1. Characteristics of Recorded Cases
From January 2015 to December 2016, 81 surgical cases were recorded. Craniotomy and craniectomy cases were 58 and trephination cases were 14 (Table 2). The mean recording time was 48 min. Detachment of the camcorder did not occur during the operations. The total size of recorded files was 731.9 GB and average data ratio was 4.2 GB per 22 min. The field of view was larger than the main operation field in most cases. However, in some cases focus was displaced from the center, especially in the early period of use.
2. Image Quality
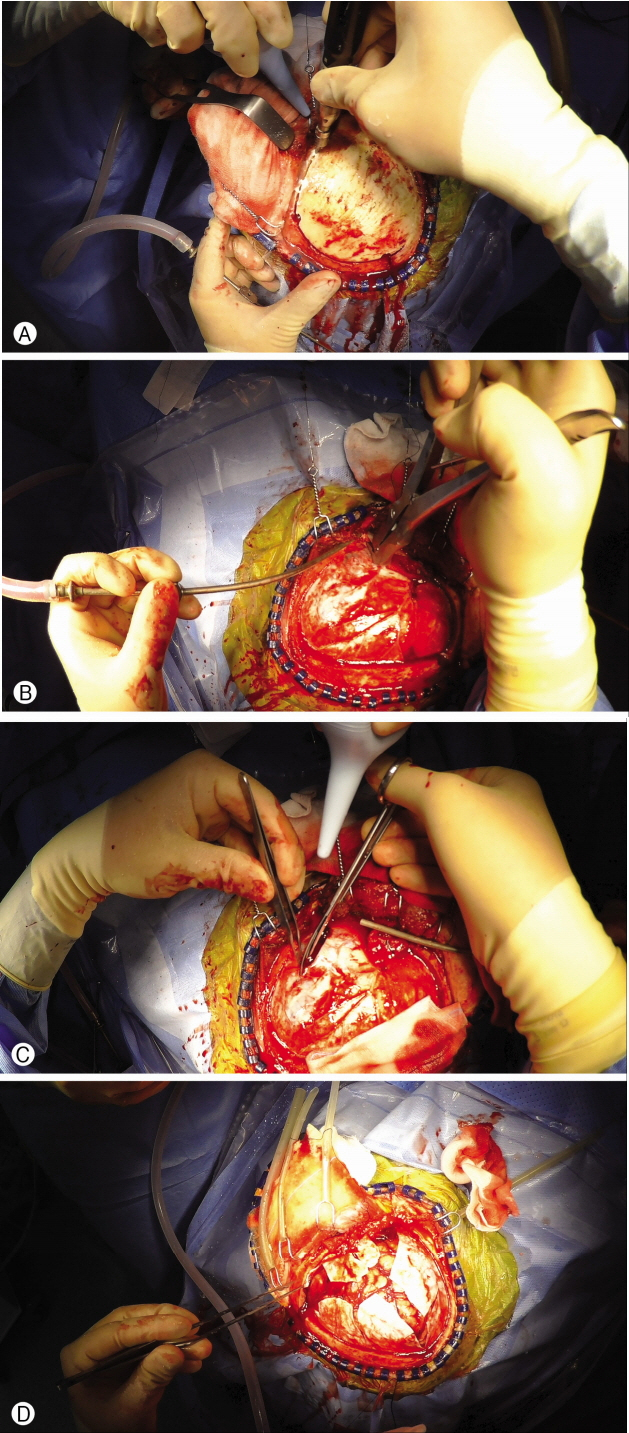
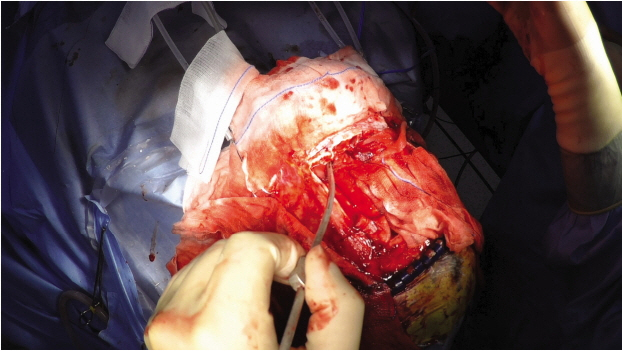
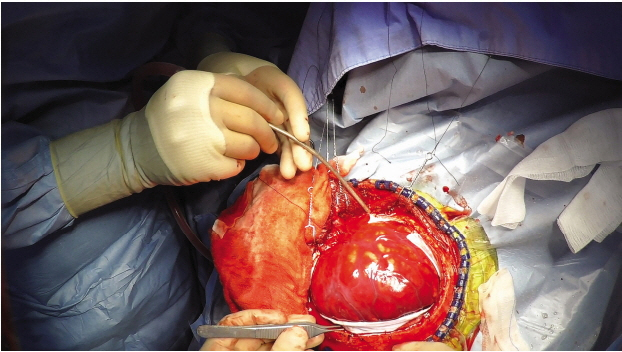
The captured video images were well identifiable. Decompressive craniectomy was easily comprehensible step by step (Fig. 2). Frontal craniotomy and frontal sinus exposure in frontal sinus fracture in patients with cerebrospinal fluid leakage were recorded (Fig. 3). After craniectomy and durotomy, swelling of the brain was recorded, including severe brain swelling, known as angry brain (Fig. 4). There were three angry brain cases. Exposure of image was controlled by the camera automatically. Overexposure caused image distortion and it happened in 5 cases. The high intensity of surgical light caused the distortion of color and detail in highlighted parts of the video. Recording time was enough to contain the most important sequence of surgery.
3. Complication and Malfunction of the Recorder
The camcorder never detached during the operations. It did not interrupt the view and movement of the assistant operator. There was no case of surgery-related infection. Unwanted camcorder shut down occurred in 2 cases and it was due to consumption of the battery. Unintended and unpredicted ceasing of recording occurred in 2 cases, because of the pressure on the buttons of the control unit during the operation.
4. Review by Residents
We selected four surgical recording movie clips. Removal of epidural hematoma, removal of subdural hematoma, decompressive craniectomy, and cranioplasty in patients with cerebrospinal fluid leakage. The 6 residents submitted their survey after reviewing the movie clips. The overall degree of help was rated at 4.26 of 5 points (Table 3). Understanding whole sequence of surgery, sharing operator’s field of view, and help for future main operators showed higher points. However, a relatively low point was seen in the handling of emergent situations.
DISCUSSION
In our study with the wearable action camera in TBI surgery recording, surgical video clips were easily obtained and had good image quality for replay and capture for still images. The battery life was less than 2 hr, but after scalp retraction, the main period of surgery was recorded in most cases. After adaption of the head mount position, out of center was rarely identified in the review.
1. Properties of Wearable Action Camcorder Necessary for Recording during Surgery
Simple control, such as start and stop recording was possible by pushing the button on the device, but real-time Wi-Fi transmission of image needed another device, such as a tablet personal computer or smartphone. This part of the procedure may need covering of aseptic pouch or another person to control it. Real-time image may be used for live surgery. Some devices also have voice command functions3,6,9).
Battery life is sufficient for recording the essential parts of surgery, but it cannot record the full length of the operation from opening to closure of the incision. If there are consecutive surgeries, not enough recording time is available without changing the battery. Since the wearable camcorders are not expensive, a second device during recording or a device with a rechargeable battery can be obtained.
Nakhla et al.10) reported on the usefulness of Google Glass (Google Inc, Mountain View, CA, USA) in surgical education of neurosurgery residents. We used a camera and body separated model. As most other devices are one-body structure, and head-mounting may cause headache or neck pain in the surgeon. An eyeglass-type recording device may reduce these disadvantages, but the image quality of current models is low and have shorter battery time6,9,10).
Surgical lighting is important for the recording image quality due to the performance of the action camera. High-intensity light may cause overexposure in most digital recording devices. We experienced some overexposed cases in the early period of recording. Before recording, it is better to lower the intensity of light for better image quality.
The technology needs to be improved to make future devices of smaller size and lighter weight, with higher image quality. They should also be able to record for longer times with extended battery life. High-quality image transmission via a wireless network, as well as real-time interaction, should be possible from the device itself.
2. Education with Surgical Video Clips
Surgery videos, recorded in this manner, may help to train neurosurgery residents and contribute to the further development of a surgeon himself. Safety of the patients and prognosis will be improved. In the past years, surgical recording needed manpower, expensive equipment, and preparation before surgery. In most TBI surgeries done in emergent or urgent situations, participating chance may not be equal in every trainee. High-quality video clips will help every trainee to learn about the surgery. We assessed the usefulness of surgical video clips in TBI surgery by surveying the residents. Residents had the experience of a main operator, and were aware of dynamic changes during surgery, and how to handle to it. Practical experience provides better understanding than textbooks and visualization of the experience of established medical professionals assists trainees in getting acquainted with their medical fields. The power of video recording in medical fields has been reported and suggested7). Microscopic or laparoscopic surgeries have incorporated video clips in most cases and they were helpful for resident or junior surgeon training4,5). TBI surgery is done as an emergent surgery in most cases. Since it is difficult for new trainees to directly perform such crucial surgeries without experience, these video recordings contribute to their learning process
CONCLUSION
We presented digital image recording in the field of neurotrauma surgery using the wearable camcorder system. It produced relatively high-quality images which provided important data for clinical practice, teaching, and preparing presentations. It is necessary to improve these small digital recording devices and use more widely in the surgical field.