INTRODUCTION
Schwannomatosis is a form of neurofibromatosis (NF) that is clinically and genetically distinct from NF type 1 (NF1) and NF type 2 (NF2). It is defined as the presence of two or more non-intradermal schwannomas, at least one with pathological confirmation, including absence of bilateral vestibular schwan noma on high-quality brain magnetic resonance imaging (MRI) and no known NF mutation4). Schwannomatosis is rare disease, having an annual incidence of 0.58 cases per 1,000,000 persons, with approximately 20% of cases being familial1).
It is commonly believed that schwannomas are derived from the nerve sheath. Cases of intraparenchymally located schwannomas in the central nervous system are very limited2,7-9). Moreover, intracerebellar schwannoma in patients with schwannomatosis is extremely rare. We present a case of intracerebellar schwannoma verified by pathological diagnosis in a patient with presumed schwannomatosis.
CASE REPORT
A 31-year-old man was admitted to our neurosurgical department with a 6-month history of progressive headache and vomiting. He was neurologically intact, and there were no cutaneous or skeletal signs of NF. He did not have any family history of NF and schwannomatosis.
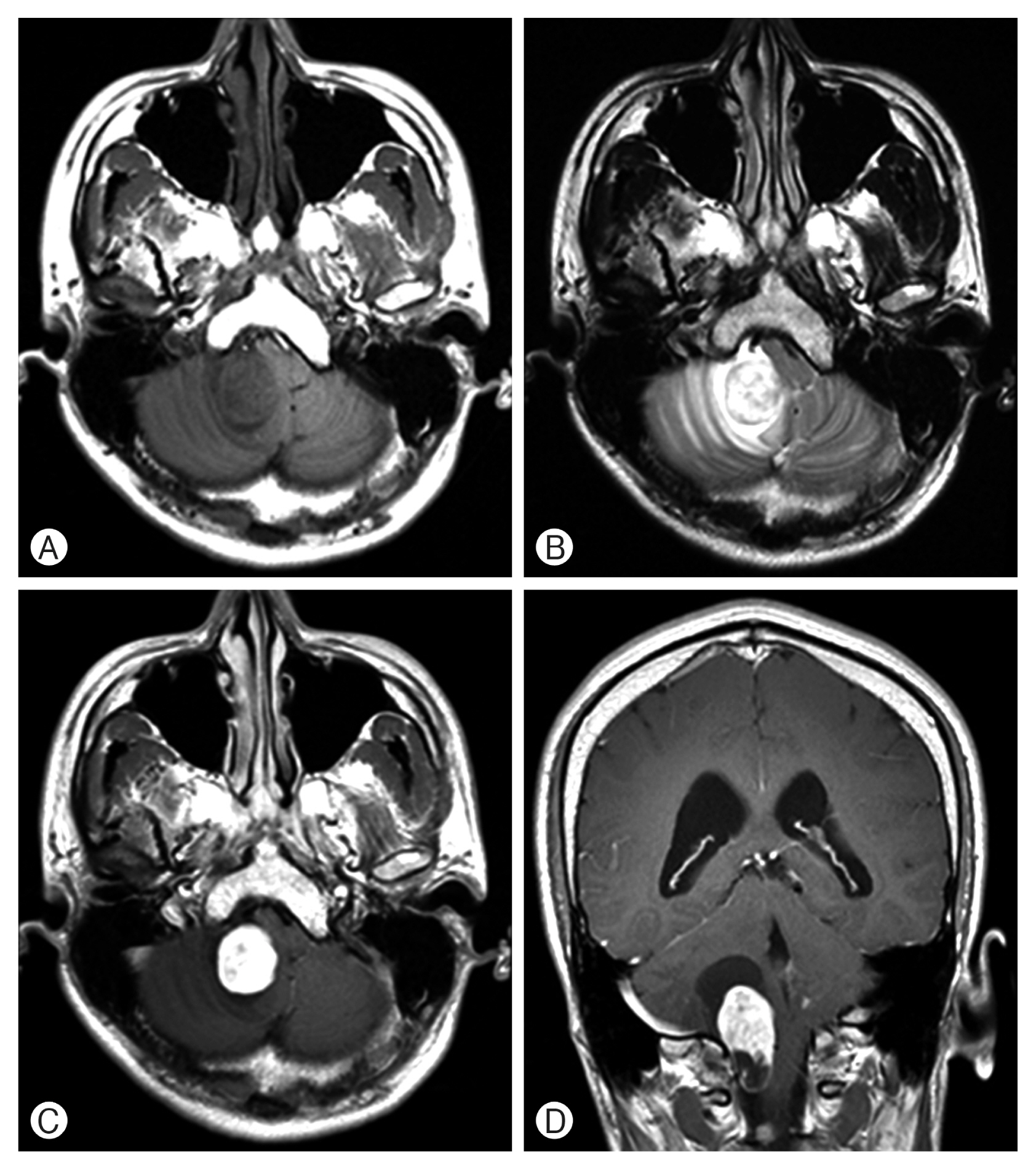
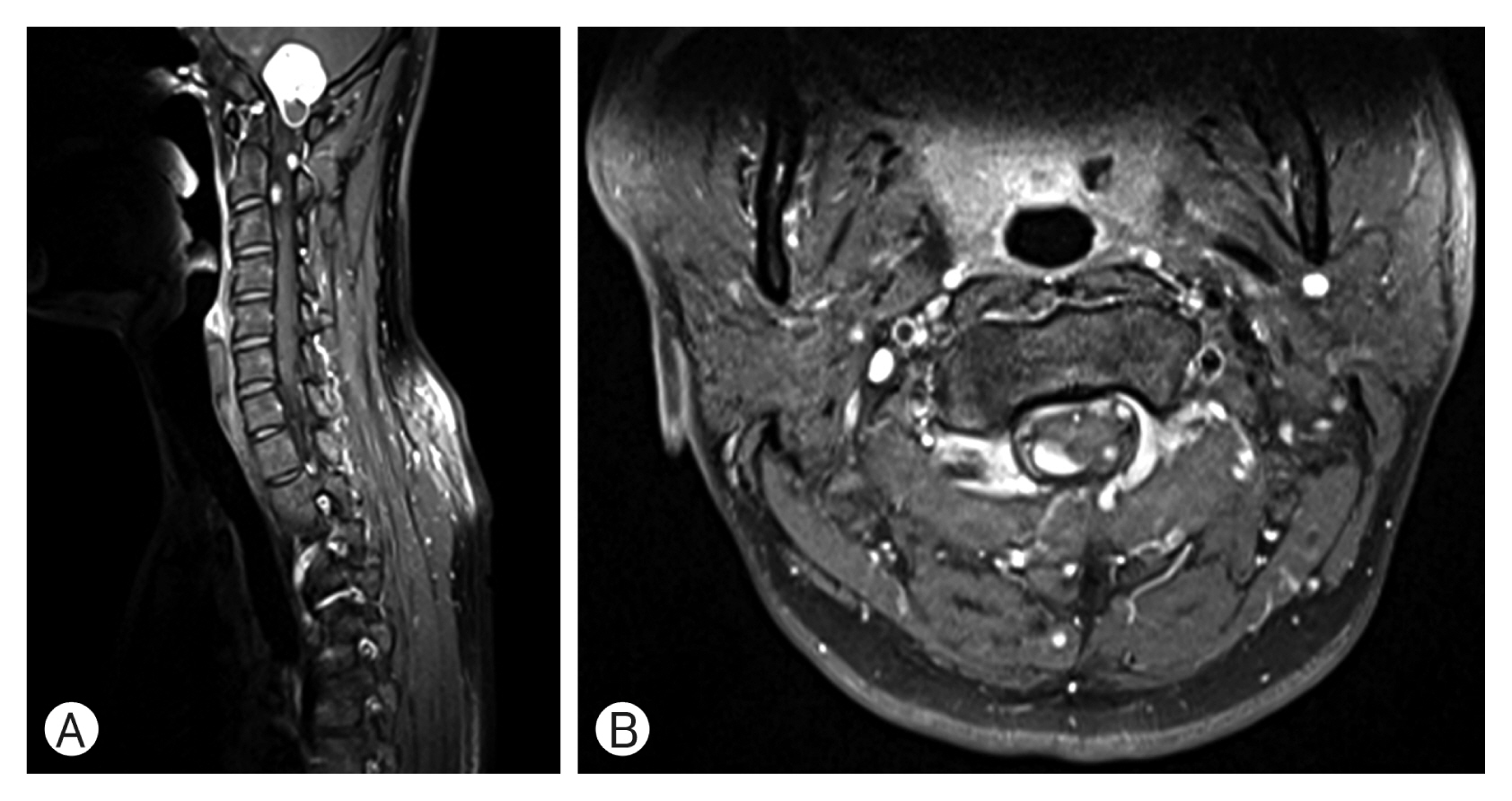
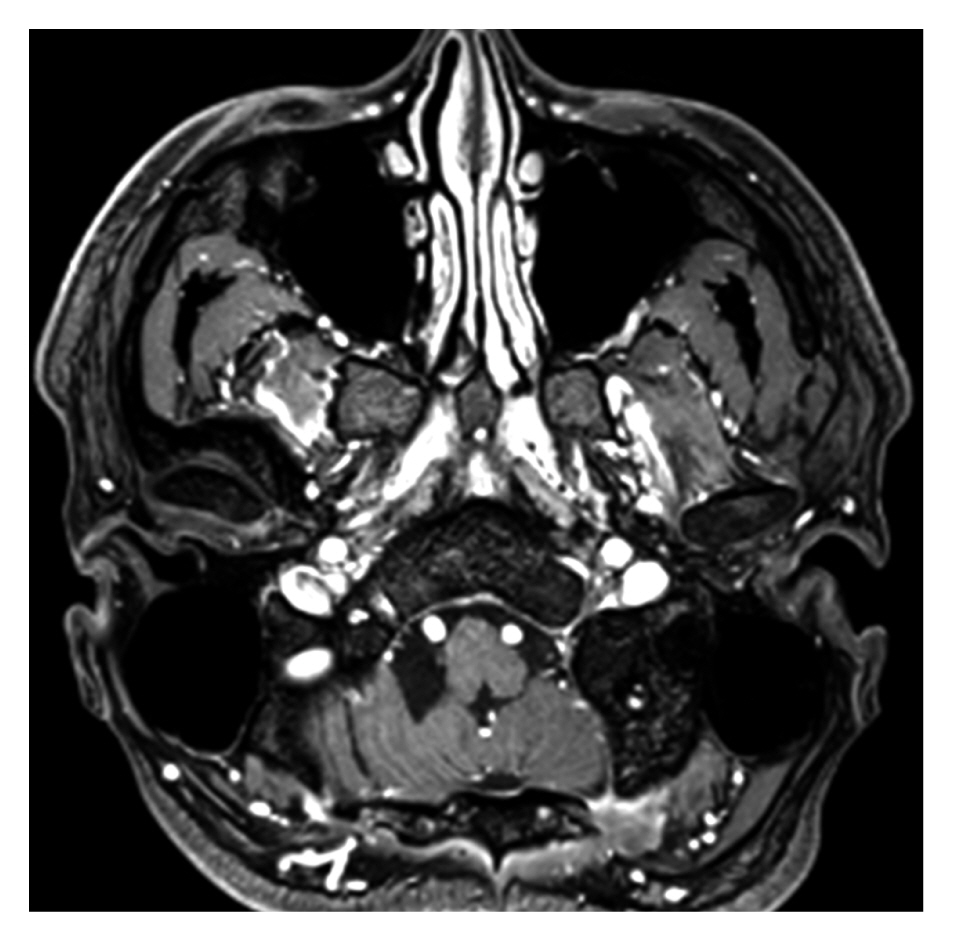
Brain computed tomography (CT) revealed a low-attenuation and round-shaped lesion in the right cerebellum. MRI revealed a round-shaped lesion in the right cerebellum with a clear margin and low signal intensity on T1-weighted imaging (WI; Fig. 1A), and non-uniform, high signal intensity on T2-WI (Fig. 1B). In contrast-enhanced MRI, a homogeneous, enhanced solid portion and a non-enhanced cystic portion were verified (Fig. 1C, D). Compression of the fourth ventricle and brain stem, and mild hydrocephalus were identified. In whole-spine MRI, multiple well-enhanced intradural extramedullary nodular lesions involving levels C1 to C3, C5 to C6, T6, and L2 to L5 were verified (Fig. 2A, B). Chest and abdominopelvic CT were performed and there was no evidence of a primary tumor or metastasis. The differential diagnosis was ependymoma with leptomeningeal metastasis versus multiple hemangioblastomas. Transfemoral cerebral angiography was performed and there was no definite tumor staining.
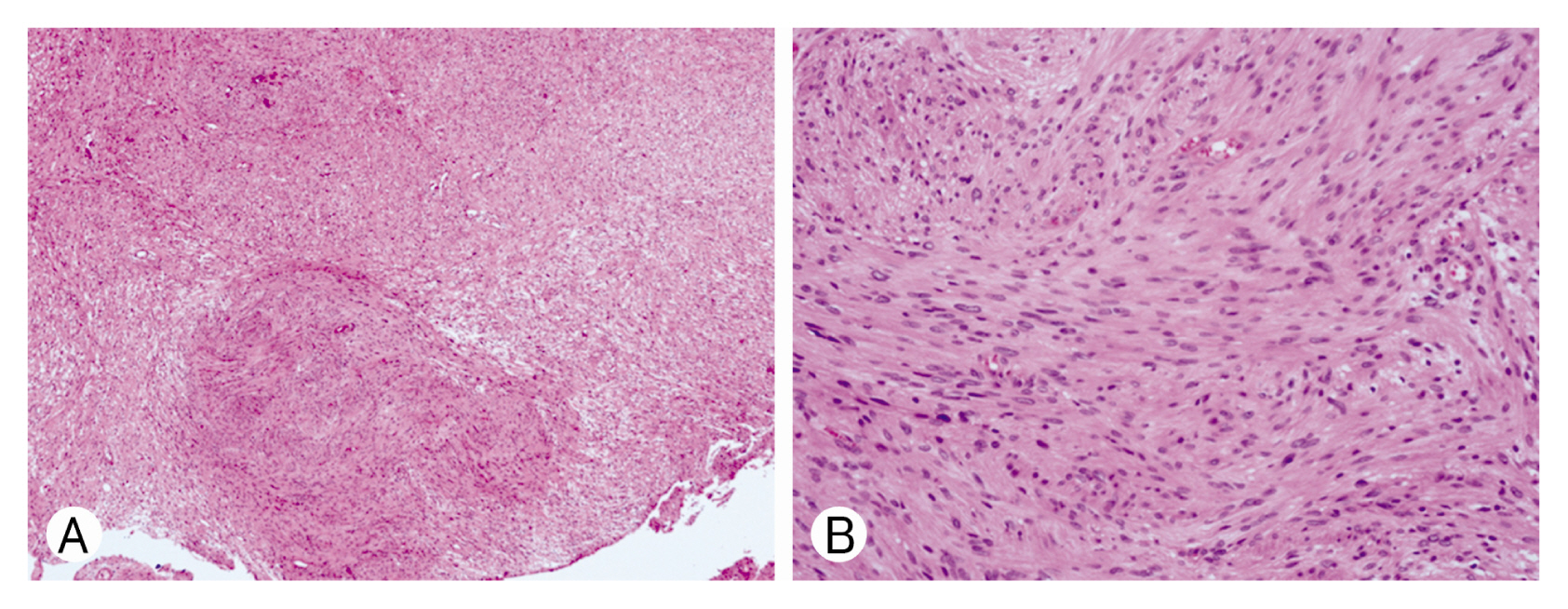
Because of hydrocephalus with brain tumor, endoscopic third ventriculostomy was initially performed, followed by midline suboccipital craniotomy and removal of the tumor. During surgery, we found that the tumor was located under the right cerebellar hemisphere cortex and had no obvious relationship with the surrounding dura and cranial nerve. The postoperative course was uneventful. His headache had resolved by the time of discharge. The tumor was diagnosed as a schwannoma (Fig. 3); hence, he was thought to have schwannomatosis. Microscopic examination revealed that the tissues were formed by spindle cells with elongated nuclei and fibrillated cytoplasm. However, due to financial constraints, molecular analysis could not be conducted. He has been followed up for more than 1 year and his condition has been stable so far. Follow-up brain MRI has revealed no recurrence (Fig. 4).
DISCUSSION
Intraparenchymal schwannomas are very rare and some cases of intracerebellar schwannomas have been reported previously. We found that in less than 20 cases, the schwannoma was located in the cerebellar hemisphere5). However, confirmed schwannoma within the cerebellum in presumed schwannomatosis is rare. In the case presented here, the diagnosis of schwannomatosis could not be confirmed because the patient was not tested for the NF mutation due to financial constraints, but schwannomatosis was very likely because he had all the other features consistent with a diagnosis of schwannomatosis. Until recently, there have been no reports of confirmed intracerebellar schwannoma in patients with schwannomatosis.
The mechanism underlying the development of intraparenchymal schwannomas remains unknown; however, several theories have been proposed. Prakash et al.6) stated that myelinated fibers with Schwann cells may be incorporated within the substance of the brain as a hamartomatous malformation, thus forming a nidus for the growth of an intraparenchymal schwannoma. Feigin and Ogata3) suggested that Schwann cells may originate from the differentiation of multipotential mesenchymal elements within the central nervous system.
Intracerebellar schwannomas are very rare tumors; however, they should be considered as differential diagnoses when a well-circumscribed nodule in the cerebellar hemisphere with typical signs of schwannomas is present in patients with schwannomatosis.
CONCLUSION
To our knowledge, this case report is the first to describe an intracerebellar schwannoma in presumed schwannomatosis. This indicates that intracerebellar schwannoma should be considered as a differential diagnoses when a nodule in the cerebellar hemisphere in patients with schwannomatosis.