INTRODUCTION
Cerebrospinal fluid (CSF) leakage is a rare complication that can occur in spinal surgery. Postoperative CSF leakage can induce delayed healing, wound infections, and intracranial hypotension, which causes neurological symptoms such as postural headache, vomiting, and dizziness3,5,11-13). Repair of CSF leakage due to dural defects that may occur during surgery is very important and Dural Sealant System can be used in this case. DuraSeal® (Integra LifeSciences, Princeton NJ, USA) is used to repair dural defects incurred during surgery and is a proven product approved by the U.S. Food and Drug Administration (FDA) in 20051,5). Several cases of spinal cord compression caused by DuraSeal® have been reported. We report a rare case of DuraSeal® causing cord compression during thoracic surgery due to dural defects. This report further supports that DuraSeal® may compress the spinal cord and lead to neurological symptoms.
CASE REPORT
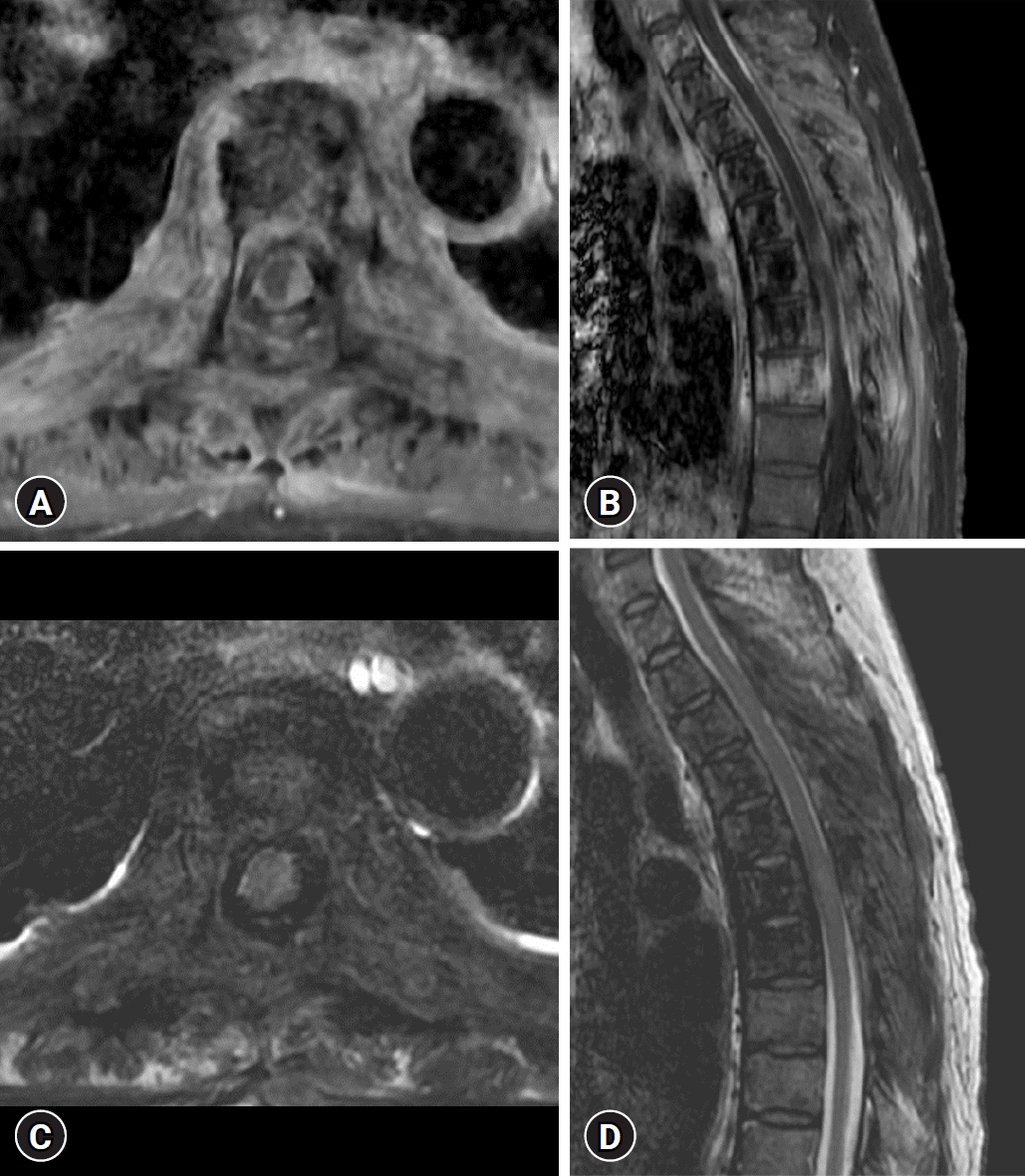
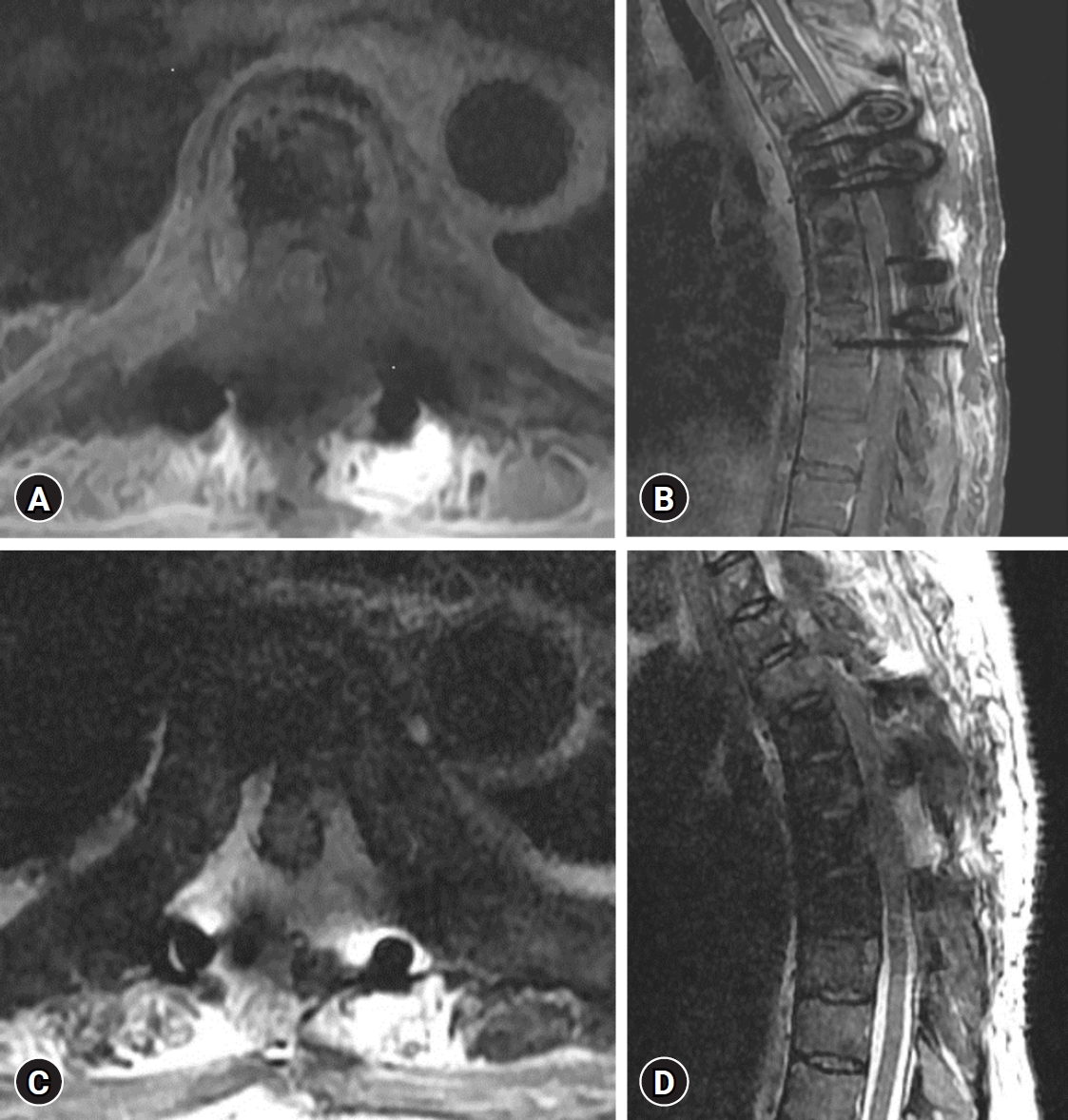
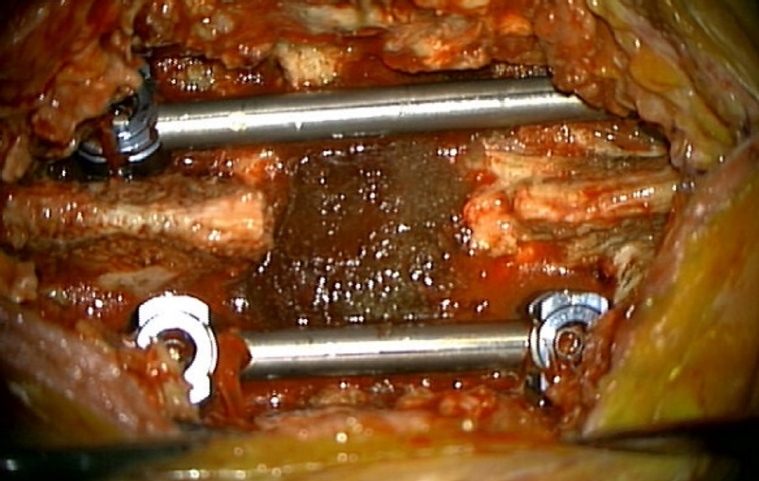
A 57-year-old female patient who was hospitalized in the hematology-oncology department due to breast cancer was transferred to the neurosurgery department for treatment after spinal metastasis was confirmed on magnetic resonance image (MRI) performed due to lower motor weakness. On physical examination, she had both lower extremity weakness (Medical Research Council [MRC] grading 4/5) and gait disturbance. MRI showed overall contrast enhancement in the range from T1 to T8 level, including the paravertebral, vertebrae body, epidural, and spinous processes, resulting in central canal stenosis, and especially cord compression due to the epidural mass effect at the T6 level (Fig. 1). The tumor removal through T6 laminectomy and T4 to T8 screw fixation was performed. The tumor was totally removed, but there was severe adhesion to the dura and there was a tear in the dura bilaterally. Dural sutures were made to repair the torn dura, and DuraSeal® was applied after sealing the dura surface with TachoComb, a patch-type hemostatic agent. The histopathologic finding was metastatic carcinoma. One day after surgery, the patient's both lower extremity weakness worsened (MRC grading 1/5). An MRI was performed immediately, and it was confirmed that an epidural mass showing a high signal on the T2-weighted image was compressing the spinal cord at the tumor removal site (Fig. 2). The patient underwent emergency wound exploration and decompression. When the wound was opened, the DuraSeal® was exposed and the cord was compressed severely (Fig. 3). DuraSeal® was removed totally, and no hematoma or CSF was seen (Fig. 4). One day after the second surgery, the patient showed improvement in both lower extremity weakness (MRC grading 2+/5).
DISCUSSION
As mentioned earlier, CSF leakage is one of the rare complications that can occur after spinal surgery5). The healing period of surgical areas such as muscles, skin, and bones may be prolonged due to CSF leakage. This can potentially lead to complications such as meningitis, nausea, vomiting, vertigo, tinnitus, postural headache, and fistula formation3,5,13). Therefore, preventing CSF leakage is very important. There are two main ways to repair CSF leakage. It is a direct repair method that repairs dural defects using an absorbable suture line and grafting fat, muscle, and fascia, or an alternative method is repaired by applying a material such as DuraSeal® to the dural defects3,13).
DuraSeal® has been approved as a synthetic sealant by the FDA and is used to promote watertight repair of dural defects that occur after neurosurgery4,5). DuraSeal® is a nontoxic bioabsorbable compound based on polyethylene glycol (PEG) and trilysine, a small amino acid. When PEG is mixed with trilysine, the substances undergo cross-linking almost instantly, resulting in the formation of a flexible layer that adheres to surrounding tissues. it also is broken down through hydrolysis over a period of 4 to 8 weeks, and the resulting byproducts are eliminated through renal clearance. Additionally, the MRI imaging characteristics of DuraSeal® are difficult to distinguish from those of CSF3,5,7,8,10).
As a characteristic of DuraSeal® shown in our case, it applied after surgery can swell by up to 50%, reaching peak expansion within 3 to 14 days, and it can last for almost four weeks3,5,9,13). Due to these characteristics, DuraSeal® may cause worsening of neurological symptoms such as postoperative quadriparesis, quadriplegia, and cauda equina syndrome2,5,6,13). We found cases of spinal cord compression after DuraSeal® application during spinal surgery reported since 2009. These are summarized in Table 1.
In the case summarized in Table 1, DuraSeal® was applied to a dura tear that occurred during surgery, and motor weakness and cauda equina syndrome subsequently occurred. The above symptoms had a latency period from immediately after surgery to 9 days, which was consistent with the peak expansion period of DuraSeal®, which was 3 to 14 days. Reoperation was performed for this, and after confirming expansion of the DuraSeal®, it was removed, and most patients' symptoms improved. Based on this, it appears that it can be inferred that cord compression occurred through DuraSeal® expansion. Additionally, in three of the reviewed cases, the hematoma at the surgical site was not properly drained due to DuraSeal® expansion. This suggests that the combination of hematoma and DuraSeal® may further compress the spinal cord1,4,13).
However, a limitation is that the absolute number of cases of side effects caused by DuraSeal® is small, and additional evaluation appears to be necessary to determine whether it is a direct effect of DuraSeal®. In the author's opinion, cord compression by DuraSeal® is likely to occur in areas where the spinal canal is limited, such as the C-spine or T-spine. However, as symptoms were reported in the L-spine as shown in the table, the cord compression by DuraSeal® is likely to occur to some extent for each level. Additional evaluation appears to be necessary regarding the effect on compression and the amount of DuraSeal® used by the surgeon.
CONCLUSION
In our case, we reported that a dura tear that occurred during surgery was repaired by applying DuraSeal®, but cord compression occurred due to the swelling characteristics of the DuraSeal®, causing neurological symptoms. DuraSeal® is a very useful material for dural repair, but it needs to be used with caution, as in the case reports that have been reported so far and in our case. In particular, care must be taken when using it in spaces where the spinal canal is relatively limited, such as the C-spine and T-spine, rather than the L-spine. When using it, the appropriate amount to fit the limited space must be applied thinly. As a result, it is necessary for the surgeon to recognize the postoperative expansion of the DuraSeal® and prevent complications that may arise from it.