INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is a standard neurosurgical procedure used in treatment of cervical spondylotic radiculopathy [2,4,9,12,16,19,20,22]. To supplement the bone grafts, various methods of anterior cervical interbody fusion have been developed over the past 4 decades; i.e., stand alone [12], autograft and plate-screw fixation [18], cage and plate-screw fixation [7], allograft and plate-screw fixation [23].
Using autograft bone or other alternatives has shown various complication -breakage, displacement, fusion failure, donor site complication [6,8,11,14]. Especially using iliac crest autograft bone, donor site complication was associated with significant shortand long-term morbidity such as infection, pelvic fracture, meralgia paresthetica, wound hematoma, loss of sensation and especially postoperative pain in up to about 20% [3,10,17,21].
Many journals have been reported that among various methods of anterior cervical interbody fusion, allobone graft and plate-screw fixation is as effective as other methods in terms of bone fusion rate, graft stability- displacement, subsidence, implant failure [5,14,18,23].
But, of the same allobone graft and plate-screw fixation methods, journals on clinical outcomes compared in accordance with the shape of allobone spacers are rare. In this paper, we compare the clinical outcomes relating shape of allobone spacer. Also, to compare the implant stability, finite element method (FEM) was performed in accordance with the 3 allobone spacer shape.
MATERIALS AND METHODS
1. Patients
Between March 2011 and February 2014, 62 patients were enrolled among the total 95 patients treated with multi-level segmental anterior cervical fusion in our institute were retrospectively reviewed. Inclusion criteria include cervical disc disease, spondylolisthesis and segmental instability, no improvement after conservative treatment for at least 6 weeks, follow-up period for more than 12 months and 62 patients were included. Thirty-three patients who had infection, neoplastic disease, hemorrhagic disease, metabolic bone disease, ossification of the posterior longitudinal ligament, combined with posterior operation and follow-up period for less than 12 months were excluded. Enrolled 62 patients were divided into 2 groups. These 31 patients (Group A) underwent ACDF using H-beam shaped allobone cervical spacer (CGBIO, Seoul, Korea) and 31 patients (Group B) underwent rim shaped allobone cervical spacer (KBB, Seoul, Korea) combined with rigid plate and screw system.
All patients were treated using a standard Robinson and Smith’s anterior cervical approach by one neurosurgeon. After the completion of discectomy and any necessary decompression under microscope, the cartilaginous endplates were removed. Endplates were cleaned and fashioned with curettes and a high-speed pneumatic drill, and we tried to preserve the endplate as much as possible to prevent cage subsidence. After intervertebral space was widened sufficiently using Caspar screw, an appropriate-size allospacer packed with demineralized bone matrix (Integra, Carlsbad, CA, USA) was inserted without impact on the spacer itself to avoid the breakage or crack. And then a rigid anterior cervical spine plate (DePuySynthes, Warsaw, IN, USA) was applied in all cases. After removing Caspar screw, anterior plate was fixed by the method that fixing screws to upper and lower level were achieved upward and downward respectively to oblique direction of the vertebral bodies. Before closing the superficial layers, a lateral radiograph was obtained, and the correct position of the implant and overdistraction was checked by comparison with the preoperative image. All patients were treated with the same protocol after surgery and consisting of immobilization with the Philadelphia cervical collar for 3 to 4 weeks.
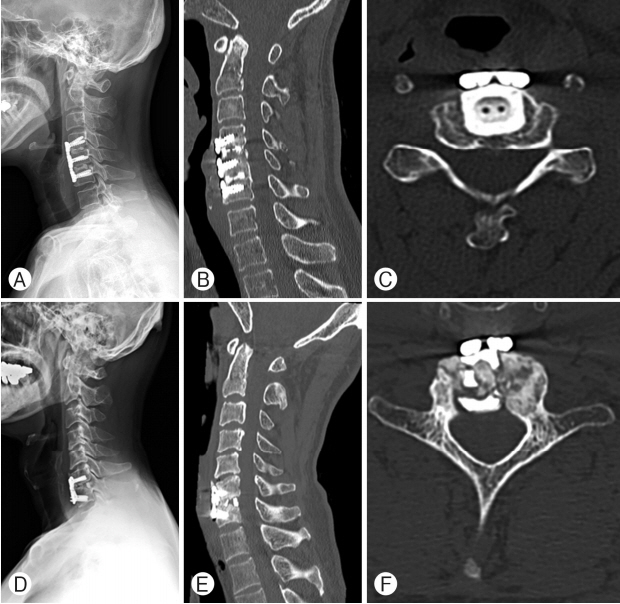
All patients were followed-up via serial cervical plain radiographs (serial anteroposterior and lateral image) and observation of clinical outcomes 3, 6, and 12 months postoperatively. Lateral flexion-extension radiography and computed tomography scan was performed for all patients to 12 months after surgery to evaluate bone fusion. Bone fusion was deemed to have occurred if visualization of trabecular bridging across the bone-graft interface, absence of radiolucent gaps between the endplate and graft, restriction of motion (0-2 mm) of the fused-level spinous process on flexion-extension.
A definition of subsidence in terms of spinal biomechanics is presented in the paper. Subsidence is defined as sinking of a body with a higher elasticity modulus (e.g., graft, cage, spacer) in a body characterized by a lower elasticity modulus (e.g., vertebral body), resulting in 3 dimensional changes of the spinal geometry [13]. Subsidence was defined as a decrease of 3 mm or more of anterior or posterior disc height from that measured on the immediate postoperative radiograph. Any excessive subsidence decreases the interbody space and produces both segmental and general kyphotic change of the spine. This may cause destabilization of the screw-plate and/or screw-bone interfaces (e.g., pulling-out, altered angulation or breakage of the screws).
A definition of spacer breakage was defined as definite recognition of linear fracture or fracture particles of allospacer on postoperative radiograph during postoperative follow-up period.
We estimated clinical outcomes such as neck and arm pain (visual analogue scale [VAS] score), radiographic fusion rate, breakage and displacement. Statistical significance was used for the Fisher’s exact test.
2. Statistical Analysis
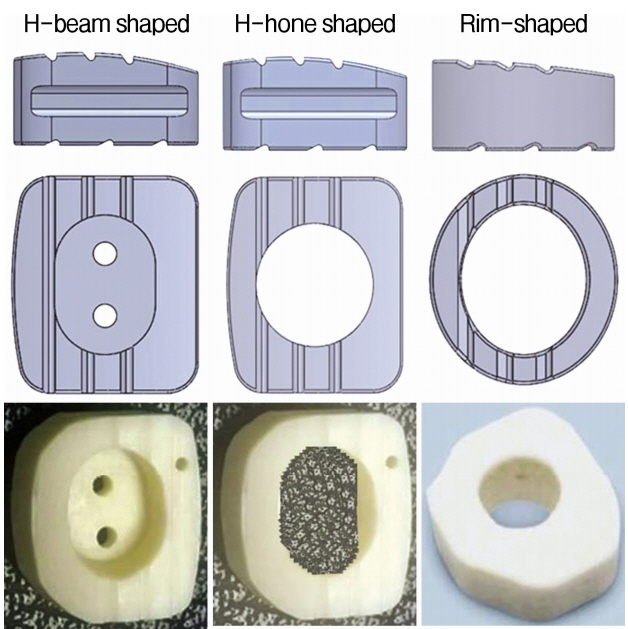
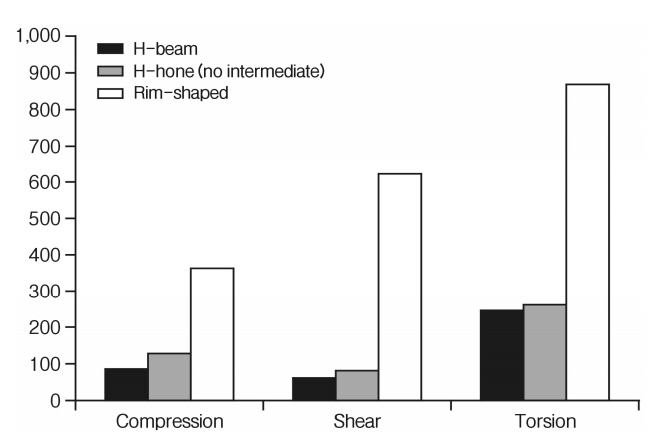
In the FEM study, we compared the implant stability of 3 different shaped allobone cervical spacer; i.e., H-beam shaped, H-hole shaped, rim-shaped (Fig. 1). We tested the effectiveness of stress distribution from the 3 types of allospacer, using the evaluation criteria of (a) compression; (b) shear; and (c) torsion, under the same load. We implemented FEM study environment according to the standards of American Society for Testing and Materials (ASTM) F-2077. In FEM study, compression, shear, torsion was set to load condition of each 2,000 N, 3 Nm, 2,000 N. Under the same load, the simulation was conducted using a jig of stainless steel material in the upper and lower implant.
RESULTS
Thirty-one patients were enrolled in Group A and underwent ACDF using H-beam shaped allobone spacer; 10 patients had a 1-level fusion, 19 patients had a 2-level fusion and 2 patients had a 3-level fusion. Thirty-one patients were enrolled in Group B and underwent ACDF using rim shaped allobone spacer; 18 the patients had a 1-level fusion, 7 patients had a 2-level fusion 6 patients had a 3-level fusion (Table 1). The mean age in each group were 54.4±13.1 years in Group A and 52.6±11.7 years in Group B. There were no statistically significant differences in age, sex ratio, follow-up period, and inclusion criteria between the groups. Diabetes mellitus and T-score of bone
mineral density (BMD) were investigated among factors that could affect implant failure, such as breakage or displacement. Those who had a history of diabetes mellitus numbered 8 in group A and 10 in group B, while the mean value of BMD was -1.6 and -2.0, respectively. However, neither showed significant differences between the 2 groups. There was statistically significant difference in surgical levels. Single level ACDF surgeries were frequently performed in Group B and multi-level ACDF surgeries (more than 2 levels) were more frequently performed in Group A. The fusion rates in the 12 months were 100% in Group A, and 96.8% Group B (Table 1). There was no significant difference in fusion rates between Group A and B (Fisher’s exact test, p>0.05) (Table 1).
We compared the complication, such as breakage, displacement of Group A and Group B. The overall breakage rates in Group A and Group B were 0% (0/31) and 16.1% (5/31), retrospectively. The incidences of defined subsidence in Group A and Group B were 0% (0/31) and 16.1% (5/31), retrospectively which were exactly same as those of breakage (Table 2). The breakage rate among patients who experienced in H-beam shaped spacer was significantly less likely than that using rimshaped spacer (Fisher’s exact test, p<0.05). There was no particular problem when using the H-beam shaded spacer, but we could see that breakage occurs when using the rim-shaped spacer. The bone fusion between the upper and lower vertebrae was good, and the plate and screw looked stable in Group A patient. Bone fusion was relatively good in Group B, but the plate and screw looked unstable (Fig. 2). The overall displacement rates in Group A and Group B were 0% (0/31) and 3.2% (1/31), respectively. The displacement rate among patients who experienced in H-beam shaped spacer was not significantly less likely than that using rim-shaped spacer (Fisher’s exact test, p>0.05) (Table 2).
We investigated the VAS for the preoperation and postoperation neck pain and arm pain. Neck pain was reduced in Group A and Group B by 68% and 73%, respectively. Also, arm pain was reduced in Group A and Group B by 63% and 72% respectively. In the VAS score, Group B is a slightly better result than the Group A (Table 3).
In FEM study, compression was set to load condition of each 2,000 N in the simulation. Under the same load, peak von mises stress (PVMS) values were checked to each 90.8 MPa, 126.3 MPa, 365.1 MPa in H-beam, H-hole, rim shaped allobone spacer. In the shear condition setting to 3 Nm, PVMS values was measured to each 61.2 MPa, 85.0 MPa, 621.2 MPa in 3 shaped allobone spacer. In the torsion condition setting to 2,000 N, PVMS values was measured to each 244.7 MPa, 261.9 MPa, 863.7 MPa in 3 different shaped spacers (Fig. 3).
DISCUSSION
As many journals have been published, in cervical interbody grafts, allograft has the effectiveness as well as other material [5,14,15,18,23]. Also, allograft is currently used in the clinic of the authors. But as it mentioned in many journals, allobone cervical spacer intermittently showed complications such as breakage, displacement also in our hospital. In this study, to reduce these complications, we compared the clinical outcomes relating shape of allobone spacer (H-beam shaped or rim shaped).
First, numerous studies have concluded that ACDF with allograft derives clinically satisfactory results in patients with cervical radiculopathy and myelopathy [1,6]. The results of this study ensure this conclusion. As seen in postoperative VAS score, H-beam shaped allograft with ACDF results in substantial pain relief, improvements in quality of life likewise rim-shaped allograft with ACDF.
Second, the displacement rate among patients who experienced in H-beam shaped spacer was not significantly less likely than that using rim-shaped spacer (Fisher’s exact test, p>0.05). It is estimated that there are associated with the surface appearance of H-beam spacer. The surface of the H-beam spacer has textured grooves. These grooves can minimize the risk of migration and displacement in anterior-posterior direction. Also, convex superior surface enhances anatomical interface with vertebral endplate-anatomical shape matches vertebral endplate. This shape confirms to anatomy of cervical vertebral bodies and minimizes tissue deformation and damage.
Third, the fusion rate at 12 month follow-ups were no significant difference in fusion rates between H-beam shaped and rim shaped allograft (Fisher’s exact test, p>0.05). It is considered that there are associated with the hole appearance of H-beam spacer. Large central hole accommodates osteobiologic material packing and promotes fusion through the implant, and the bed of central hole can minimize the risk of migration that it is caused by the force of gravity in inferior direction. Also, 1 mm pattern holes promote fusion through the implant and help blood circulation.
Forth, the breakage rate among patients who experienced in H-shaped spacer was significantly less likely than that using rim-shaped spacer (Fisher’s exact test, p<0.05). Single level ACDF surgeries were frequently performed in Group B and multi-level ACDF surgeries (more than 2 levels) were more frequently performed in Group A. Even though 5 patients in Group B showed breakage of allospacer, only 1 patient needed to have additional surgery because of fusion failure. Reinforcement using plate and screw system could give additional stability in spite of the breakage of the allospacer, and so fusion rate between groups was not statistically significant. But, the cases of allospacer breakage showed statistically significant difference (Fisher’s exact test, p<0.05).
H-beam shaped spacer showed better result than rim shaped spacer in the breakage. We have conducted a FEM study to find the systemic and biomechanical cause for these results. We designed the 3 different shaped spacer models; H-beam shaped, H-hole shaped and rim shaped. Shapes of 3 models were similarly designed to real allospacers which were being used in the current practice. In FEM study, the results were derived from 3 types of spacer that H-beam shaped allobone spacer was the most effectiveness stress distribution. Among the results, under to the compression, shear force load, PVMS values were placed on the thread value. On the other hand, under to the torsion load, H-beam shaped allospacer was showed PVMS value corresponding to 28.3% relative to other allospacer. It means that the effective stress distribution when the torsion load than the other loads. It is considered that is a great role to apply a support structure (H-shape) in the central part unlike conventional products (rim shaped allospacer). Rim- shaped allospacer was also showed a large PVMS value under the shear, torsion load. This result is thought to be the cause of a thin thickness of rim shaped allospacer. In conclusion, because of many rotary motion of cervical spine, applying a structure in the middle of the spacer is likely to give high stability.
The journals on clinical outcomes and FEM study compared in accordance with the shape of allobone cervical spacers are rare. Perhaps this retrospective study is considered to be the first study comparing the clinical outcome and complication in according to the cervical spacer shape. As mention above, if clinical outcomes and FEM study results is changed in accordance with the cervical spacer shape, we can see that the consideration of the spacer shape is required
However, a limitation of this study is that the 2 groups were not randomly selected for treatment, and thus the groups are not strictly comparable. Another limitation is the small number of patients in each group. Also this study has the limitation of FEM study, not clinical trial.
CONCLUSION
Cervical allospacer and plate-screw fixation is stable fusion rate with low incidence of complications compared with those of other cervical implants. In ACDF using allograft, H-beam shaped allospacer shows stable fusion rate with low incidence of complication compared with those of other types of allospacer.