AbstractObjectiveThromboembolism is the most common complication in stent-assisted coiling (SAC) procedures. This study aimed to evaluate the incidence and risk factors of thromboembolic complication in patients who underwent SAC for intracerebral aneurysm.
MethodsBetween January 2006 and December 2017, 35 patients (35 aneurysms) in the acute phase of subarachnoid hemorrhage (SAH) underwent SAC without antiplatelet premedication. Additionally, 45 patients (48 unruptured aneurysms) underwent SAC with antiplatelet premedication. Baseline patient characteristics were compared between the unruptured and ruptured aneurysm groups. Risk factors of thromboembolic complications were also analyzed.
ResultsThromboembolic complications occurred in 11 of 83 aneurysms treated with SAC, among which 3 occurred in 48 unruptured aneurysms (6.3%; p=0.046) and 8 occurred in 35 ruptured aneurysms (22.9%; p=0.046). However, there was no permanent morbidity due to thromboembolic complications in either group.
ConclusionThe thromboembolic complication rate for SAC in patients with ruptured aneurysms was significantly higher than for those with unruptured aneurysms. However, there was no permanent morbidity of thromboembolic complications, there seems to be no reason to reluctant SAC due to the risk of thromboembolic complications in patients with SAH.
INTRODUCTIONStent-assisted coiling (SAC) is one of the most commonly used neck remodeling techniques for wide-necked aneurysms [5,6,10,25,27]. Development of the stent has led to easier and more effective treatment of many complex aneurysms [1,4,16,24]. There are also many strategies and methods to treat difficult aneurysms by using stents, with or without coil embolization [18]. Although SAC has expanded the scope of aneurysms treatment options, thromboembolic complication in SAC has been reported with an incidence of 2.3% to 20% [3,7,11,12,22].
Dual antiplatelet medication is frequently administered in intracranial stent procedures to prevent thromboembolic complications. Patients are routinely prescribed perioperatively and maintained with dual antiplatelet medication over 6 months to prevent in-stent thrombosis. The use of dual antiplatelet medication limits SAC in patients with subarachnoid hemorrhage (SAH). Most operators are reluctant to use dual antiplatelet therapy in acutely ruptured aneurysms due to the potential for rebleeding and additional invasive procedures [2,19]. Therefore, stent placement is generally avoided in acutely ruptured aneurysms in favor of clip ligation or other endovascular techniques that do not mandate dual antiplatelet therapy [12,26].
In this retrospective study, we evaluated the incidence of thromboembolic complications in patients who underwent SAC for acutely ruptured aneurysms without antiplatelet premedication. In addition, we compared the thromboembolic complication rates with those of unruptured aneurysms treated with stent assistance and anti-platelet premedication during the same period. We also analyzed predictors for thromboembolic complications.
METERIALS AND METHODS1. Patient PopulationThe Institutional Review Board of the author’s hospital approved this study and waived requirements for informed consent due to its retrospective observational design and the use of anonymized patient data. Between January 2006 and December 2017, 662 patients with 675 aneurysms were treated using endovascular techniques. A total of 587 aneurysms treated with coiling alone and 5 patients with unruptured aneurysms who underwent SAC without appropriate premedication were excluded. Thirty-five aneurysms in 35 patients who underwent SAC in the acute phase of SAH without antiplatelet premedication, and 48 unruptured aneurysms in 45 patients who underwent SAC with antiplatelet premedication, were included in the analysis (Fig. 1). Demographic information, medical comorbidities, aneurysm characteristics, and clinical features of the patients on admission were documented.
2. Indications for SACIndications for SAC included wide-necked aneurysms, dissecting aneurysms, and coil protrusion. Wide-necked aneurysms were defined as aneurysms with a fundus-to-neck ratio of <2 or a neck width >4 mm.
3. Premedication and Intraprocedural Medication ProtocolPatients with ruptured aneurysms were not medicated with antiplatelet agents before procedure. When a stent was placed, dual antiplatelet drugs with a loading dose (clopidogrel 300 mg and aspirin 400 mg) were administered orally or through a nasogastric tube immediately after the procedure, followed by clopidogrel 75 mg and aspirin 100 mg daily. Patients with unruptured aneurysms were preloaded for 5 days with clopidogrel 75 mg and aspirin 100 mg daily, and were heparinized during the procedure. Dual antiplatelet therapy was continued for 6 months, in addition to aspirin 100 mg daily, life-long. Response to antiplatelet therapy was tested before the procedure.
Patients with unruptured aneurysms were systemically anticoagulated with intravenous heparin at the beginning of the procedure with initial boluses of 100 U/kg, followed by continuous infusions of 10 U/kg/h. Patients with ruptured aneurysms received intravenous heparin after deployment of the frame coil or stent. In the event of a periprocedural thromboembolic complication, Tirofiban (Aggrastat; Medicure Pharma, Somerset, NJ, USA) was slowly injected intra-arterially with a loading dose of 500 mcg/10 mL, continued intravenously at an initial rate of 0.4 mcg/kg/min for 30 min, and then continued at 0.1 mcg/kg/min or used temporarily.
4. Definition and Outcome Parameter of Thromboembolic ComplicationsOnly immediate thromboembolic complications that occurred during procedure or within 24 hr after procedure were considered. Thromboembolic complications were diagnosed intraoperatively on digital subtraction angiography (DSA), clinically as new deficits or change in level of consciousness, or on diffusion-weighted imaging (DWI) (new infarcts) performed in cases of sudden neurological compromise. Patient outcomes assessed at discharge using modified Rankin scale (mRS). We defined a poor score as mRS ≥3.
5. Statistical AnalysisBaseline patient characteristics, aneurysm characteristics, and procedure duration were compared between the unruptured and ruptured aneurysm groups. Variables were analyzed using the χ2 test and the Student’s t-test, as appropriate. All p-values of less than 0.05 were considered to indicate statistical significance. Multivariable analyses were performed via multiple logistic regression to determine risk factors associated with thromboembolism. In multivariable analysis, variables with p<0.2 in the univariate analysis were selected as potential factors for statistical analysis. All analyses were performed using PASW Statistics version 18.0 (IBM Corp., Armonk, NY, USA).
RESULTS1. Comparison of the Unruptured and Ruptured Aneurysm GroupsClinical (age, sex, medical history, laboratory findings at the time of admission) and radiological characteristics (location, type, procedure time, and thromboembolic complications) were compared between the unruptured (n=48) and ruptured (n=35) aneurysm groups (Table 1). There were statistically significant differences in activated partial thromboplastin time (p<0.001), activated clotting time (p=0.045), procedure time (p=0.024), thromboembolic complication (p=0.046), and dissecting aneurysm (p=0.016) between the 2 groups. Thromboembolic complications occurred in 11 of 83 aneurysms that underwent SAC, among which 3 occurred in 48 unruptured aneurysms (6.3%; p=0.046) and 8 occurred in 35 ruptured aneurysms (22.9%; p=0.046)
2. Predictors for Thromboembolic Complication of SACClinical characteristics (age, sex, medical history, laboratory findings at the time of admission), procedure time, rupture of aneurysm, size and location of aneurysm were tested for as predictors of complication. In univariate analysis (Table 2), procedural time >3 hr (p=0.002) and ruptured aneurysm (p=0.046) were statistically significant predictors. The odds ratio (OR) using univariate analysis was obtained as ruptured aneurysm (OR=4.44; 95% confidence interval [CI]=1.24-68.33), age (OR=1.05; 95% CI=0.97-1.14), smoking (OR=8.5; 95% CI=1.2-60.39), and procedure time >3 hr (OR=3.29; 95% CI=1.39-7.80) (Table 3). In the odd ratio from multivariate analysis, smoking (OR=6.51; 95% CI=1.04-40.91), and procedure time >3 hr (OR=2.84; 95% CI=1.33-6.09) were statistically significant independent predictors for thromboembolic complication (Table 3).
3. Subgroup Analysis of Patients with Thromboembolic ComplicationSubgroup analysis was performed on the 11 patients who experienced thromboembolic complications (Table 4). In 9 patients, thrombus was observed on DSA; 8 patients received tirofiban in the artery, and the other patient exhibited very little thrombus and no symptoms. All 8 patients who received tirofiban exhibited successful recanalization. Two patients with no thrombus during the procedure were found new infarct on DWI performed to distinguish the cause of neurological deterioration after the procedure. Three patients with unruptured aneurysm exhibited no permanent neurological deficits. Of the 8 patients with ruptured aneurysm, 5 exhibited no permanent neurological deficits, and the other 3 died. However, all 3 patients who died were Hunt and Hass grade IV, and their respective causes of death were severe vasospasm, cardiac complications, and rebleeding due to incomplete obliteration of the aneurysm.
4. Case Description1) Patient 3A 73-year-old man with a history of hypertension and cerebral infarction was referred to our neurosurgical department for treatment of a unruptured aneurysm in the anterior communicating artery (ACoA). He had no neurological deficits. We planned endovascular treatment and the patient was preloaded for 5 days with clopidogrel 75 mg and aspirin 100 mg daily. DSA demonstrated a 3.8×4.2-mm wide-necked aneurysm at the left ACoA. As the frame coil failed to deploy, we performed SAC. Enterprise (Codman & Shurtleff, Raynham, MA, USA) stent was placed from right proximal A2 to right proximal A1. A total of 7 coils were inserted in the aneurysm sac using the jailing technique. Thrombus was observed in the left proximal A2 and aneurysm junctional area after the last coil insertion (Fig. 2A, B). After intra-arterial and intra-venous infusion of Tirofiban, the left proximal A2 was recanlized (Fig. 2C). The patient was discharged without neurological deficits.
2) Patient 7A 51-year-old man presented to the emergency room after the sudden onset of thunderclap headache. The patient had no other significant medical history and no neurological deficits except for neck stiffness on neurologic examination. A non-contrast computed tomography scan of the brain was performed immediately, demonstrating Fisher grade III SAH (Fig. 3A). The patient was rated as grade II according to Hunt and Hess scale for SAH. DSA showed a wide-necked ruptured aneurysm in the ACoA. SAC via use of the jailing technique for obliteration of aneurysm was performed due to the frame coil failed to deploy. Enterprise stent was placed from right proximal A2 to right proximal A1. During the procedure, thrombus was formed around the neck of the aneurysm, and then the right proximal A2 was completely occluded (Fig. 3B). After infusion of Tirofiban according to the protocol, the right anterior cerebral artery (A2) was recanalized (Fig. 3C). Then, using the through the stent technique, the coil was additionally inserted into the aneurysm for complete embolization. The patient was discharged without neurological deficits after 2 weeks.
DISCUSSIONSAC in unruptured aneurysms is currently accepted to be a safe treatment option. SAC enables denser aneurysm packing with increased neck coverage, and may also improve treatment durability through a combination of flow diversion, parent vessel straightening, and fibroelastic tissue formation along the neck of the aneurysm [8,10,15,20,25]. SAC provides a high rate of adequate occlusion, leading to a decrease in the recanalization rate in long-term follow up [10,23]. Several studies have demonstrated that the risk for complications in coiling using stents is not significantly higher than the risk for complications in coil-only treatments [15,22]. In the present study, none of the 3 patients who experienced thromboembolic complications among the unruptured aneurysms who underwent SAC experienced permanent morbidity.
Although the utility of SAC has been demonstrated, thromboembolic complications during the procedure and additional risks associated with antithrombotic agents have been regarded to be serious impediments to the use of stents in patients with acute ruptured aneurysms. SAH in the acute period triggers the coagulation cascade, leading to a hypercoagulable state with a high tendency for clotting or thrombosis. Interventional procedures and inserted stents activating platelet function potentially induce thromboembolism [9]. In addition, SAH patients did not undergo antiplatelet therapy before the procedure. Lessne et al. [22] reported that in patients undergoing SAC, there was a 3.1% rate of thromboembolic complications in unruptured aneurysms and 20% in those with SAH. Bechan et al. [3] compared complications of SAC in unruptured and ruptured aneurysm groups, with thromboembolism occurring in 4% and 20%, respectively. Similar to previous studies, we found that the thromboembolic complication rate for SAC in patients with ruptured aneurysms was significantly higher than that for SAC of unruptured aneurysms. Thromboembolic complications occurred in 11 of 83 aneurysms that underwent SAC, among which 3 occurred in 48 unruptured aneurysms (6.3%; p=0.046) and 8 occurred in 35 ruptured aneurysms (22.9%; p=0.046).
Generally, the incidence of thromboembolic complications is higher in patients with SAH than in those with unruptured aneurysms due to the increased coagulation cascade and absence of antiplatelet therapy before the procedure [12]. Risk factors for thromboembolic complications have been discussed in previous studies. Chalouhi et al. [10] analyzed the predictors of thromboembolic complication in 552 patients (552 aneurysms) who were treated with SAC. Acutely ruptured aneurysms (OR=2.8; 95% CI=1.1-7; p=0.01), delivery of coils before stent placement (OR=5.2; 95% CI=2-15; p=0.002), and carotid terminus/middle cerebral artery aneurysm locations (OR=3.2; 95% CI=1.2-8.5; p=0.02) were statistically significant independent predictors of complications. Cai et al. [7] studied the association between different stenting procedures and procedure-related complications of SAC for ruptured, wide-necked aneurysms. Stenting procedures using the coil-then-stent technique demonstrated a higher rate of symptomatic thromboembolic complications compared with the jailing-outside-of-the-stent and the coil-through-the-struts techniques. In this study, smoking (OR=6.51; 95% CI=1.04-40.91), and procedure time >3 hr (OR=2.84; 95% CI=1.33-6.09) were statistically significant independent predictors for thromboembolic complication.
Procedure time was defined as the time between the first and the last angiographic run, since this time period could easily be assessed from time prints on the images. Long procedure duration could be associated with the use of a device, aneurysmal size, and procedural morbidity [13]. Another previous study reported that longer procedure times may be affected by multiple procedural manipulations of each aneurysm and/or an inefficient periprocedural processes, and that reducing the procedure duration can be the most effective modifiable factor an interventionist can use to reduce the risk for thromboembolism after coil embolization of an intracerebral aneurysm [21]. If thromboembolic complications occur, several measures may be implemented, such as mechanical thrombus fragmentation and selective injection of a thrombolytic agent [13]. Tirofiban demonstrated excellent recanalization effects and satisfactory outcomes in patients with thromboembolic complications undergoing SAC [9,14,17]. In the present study, we used Tirofiban infusion in 8 patients with thromboembolic complications during SAC procedures, all of whom exhibited recanalization without hemorrhagic complications related to Tirofiban infusion.
Our study was limited by the absence of randomization of the study groups. The results reflect the experience of a single neurovascular center that uses a specific technique and anticoagulation protocols, which may not be readily generalizable to other centers. Individual responses to antiplatelet medication were not tested. Because DWI was not routinely performed, the incidence of clinically silent infarcts has likely been underestimated. Furthermore, our study was limited by its retrospective design and small sample size. Platelet function testing was not performed in all patients before antiplatelet therapy. Finally, only thromboembolic complications were examined and hemorrhagic complications were not considered.
CONCLUSIONThe thromboembolic complication rate for SAC in patients with ruptured aneurysms was significantly higher than for SAC of unruptured aneurysms. Moreover, smoking and long procedure duration were independent risk factors for thromboembolic complications in SAC. However, there was no permanent morbidity of thromboembolic complications, there seems to be no reason to reluctant SAC due to the risk of thromboembolic complications in patients with SAH.
Fig. 1.Flow chart of 675 aneurysms in 662 patients treated endovascularly between January 2006 and December 2017. 
Fig. 2.A 73-year-old man presented with a wide-necked unruptured aneurysm at the anterior communicating artery. (A, B) Thrombus (arrow) was observed in the left proximal A2 after the last coil insertion. (C) After intra-arterial and intra-venous infusion of tirofiban, the left proximal A2 was recanalized. 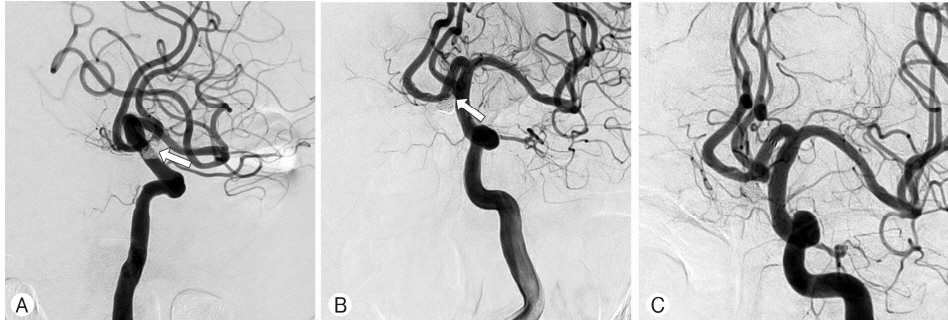
Fig. 3.A 51-year-old man presented with a Hunt and Hess grade II subarachnoid hemorrhage (SAH). (A) A brain computed tomography scan demonstrates a Fisher grade III SAH. (B) The right carotid artery angiogram during procedure demonstrates thrombus formation (arrow) and total occlusion on the right proximal A2. (C) After infusion of tirofiban according to the protocol, the right anterior cerebral artery (A2) was recanalized (arrow). 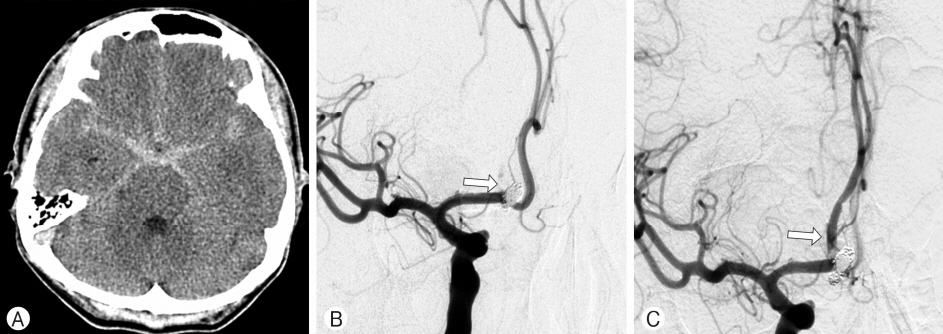
Table 1.Baseline characteristics of the unruptured and ruptured aneurysm groups
Data are presented as n (%) or mean±standard deviation. DM: diabetes mellitus; HTN: hypertension; aPTT: activated partial thromboplastin time; INR: international normalized ratio; ACT: activated clotting time; ACA: anterior cerebral artery; MCA: middle cerebral artery; ICA: internal carotid artery; BBA: blood blister-like aneurysm. Table 2.Univariate analysis for the risk of thromboembolism
Data are presented as n (%) or mean±standard deviation. DM: diabetes mellitus; HTN: hypertension; aPTT: activated partial thromboplastin time; INR: international normalized ratio; ACA: anterior cerebral artery; MCA: middle cerebral artery; ICA: internal carotid artery; BBA: blood blister-like aneurysm. Table 3.Crude odd ratio and adjusted odd ratio of the significant variable for thromboembolic complication in univariate and multivariate logistic regression analysis Table 4.Demographic and clinical data of 11 patients with thromboembolic complications M: male; F: female; BA: basilar artery; MCA: middle cerebral artery; ACoA: anterior communicating artery; VA: vertebral artery; PCoA: posterior communicating artery; ICA: internal carotid artery; BBA: blood blister-like aneurysm; DWI: diffusion-weighted imaging; SAC: stent-assisted coiling; HH grade: Hunt and Hess grade; mRS: modified Rankin scale. REFERENCES1. Akpek S, Arat A, Morsi H, Klucznick RP, Strother CM, Mawad ME: Self-expandable stent-assisted coiling of wide-necked intracranial aneurysms: a single-center experience. AJNR Am J Neuroradiol 26:1223-1231, 2005
2. Amenta PS, Dalyai RT, Kung D, Toporowski A, Chandela S, Hasan D, et al.: Stent-assisted coiling of wide-necked aneurysms in the setting of acute subarachnoid hemorrhage: experience in 65 patients. Neurosurgery 70:1415-1429, 2012
3. Bechan RS, Sprengers ME, Majoie CB, Peluso JP, Sluzewski M, van Rooij WJ: Stent-assisted coil embolization of intracranial aneurysms: Complications in acutely ruptured versus unruptured aneurysms. AJNR Am J Neuroradiol 37:502-507, 2016
4. Benitez RP, Silva MT, Klem J, Veznedaroglu E, Rosenwasser RH: Endovascular occlusion of wide-necked aneurysms with a new intracranial microstent (Neuroform) and detachable coils. Neurosurgery 54:1359-1367, 2004
5. Biondi A, Janardhan V, Katz JM, Salvaggio K, Riina HA, Gobin YP: Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms: strategies in stent deployment and midterm follow-up. Neurosurgery 61:460-468, 2007
6. Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF: Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol 32:1232-1236, 2011
7. Cai K, Ji Q, Cao M, Shen L, Xu T, Zhang Y: Association of different stenting procedures with symptomatic thromboembolic complications in stent-assisted coiling of ruptured wide-necked intracranial aneurysms. World Neurosurg 104:824-830, 2017
8. Cantón G, Levy DI, Lasheras JC, Nelson PK: Flow changes caused by the sequential placement of stents across the neck of sidewall cerebral aneurysms. J Neurosurg 103:891-902, 2005
9. Chalouhi N, Jabbour P, Kung D, Hasan D: Safety and efficacy of tirofiban in stent-assisted coil embolization of intracranial aneurysms. Neurosurgery 71:710-714, 2012
10. Chalouhi N, Jabbour P, Singhal S, Drueding R, Starke RM, Dalyai RT, et al.: Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke 44:1348-1353, 2013
11. Chitale R, Chalouhi N, Theofanis T, Starke RM, Amenta P, Jabbour P, et al.: Treatment of ruptured intracranial aneurysms: comparison of stenting and balloon remodeling. Neurosurgery 72:953-959, 2013
12. Chung J, Lim YC, Suh SH, Shim YS, Kim YB, Joo JY, et al.: Stent-assisted coil embolization of ruptured wide-necked aneurysms in the acute period: incidence of and risk factors for periprocedural complications. J Neurosurg 121:4-11, 2014
13. de Gast AN, Soepboer A, Sluzewski M, van Rooij WJ, Beute GN: How long does it take to coil an intracranial aneurysm? Neuroradiology 50:53-56, 2008
14. Dornbos D, Katz JS, Youssef P, Powers CJ, Nimjee SM: Glycoprotein IIb/IIIa inhibitors in prevention and rescue treatment of thromboembolic complications during endovascular embolization of intracranial aneurysms. Neurosurgery 82:268-277, 2018
15. Feng MT, Wen WL, Feng ZZ, Fang YB, Liu JM, Huang QH: Endovascular embolization of intracranial aneurysms: To use stent(s) or not? Systematic review and meta-analysis. World Neurosurg 93:271-278, 2016
16. Fiorella D, Albuquerque FC, Masaryk TJ, Rasmussen PA, Mc-Dougall CG: Balloon-in-stent technique for the constructive endovascular treatment of "ultra-wide necked" circumferential aneurysms. Neurosurgery 57:1218-1227, 2005
17. Kang HS, Kwon BJ, Roh HG, Yoon SW, Chang HW, Kim JE, et al.: Intra-arterial tirofiban infusion for thromboembolism during endovascular treatment of intracranial aneurysms. Neurosurgery 63:230-237, 2008
18. Kim BM, Kim DJ, Kim DI: Stent application for the treatment of cerebral aneurysms. Neurointervention 6:53-70, 2011
19. Knight CJ, Panesar M, Wilson DJ, Patrineli A, Chronos N, Wright C, et al.: Increased platelet responsiveness following coronary stenting. Heparin as a possible aetiological factor in stent thrombosis. Eur Heart J 19:1239-1248, 1998
20. Lawson MF, Newman WC, Chi YY, Mocco JD, Hoh BL: Stentassociated flow remodeling causes further occlusion of incompletely coiled aneurysms. Neurosurgery 69:598-603, 2011
21. Lee SH, Jang MU, Kang J, Kim YJ, Kim C, Sohn JH, et al.: Impact of reducing the procedure time on thromboembolism after coil embolization of cerebral aneurysms. Front Neurol 9:1125, 2018
22. Lessne ML, Shah P, Alexander MJ, Barnhart HX, Powers CJ, Golshani K, et al.: Thromboembolic complications after neuroform stent-assisted treatment of cerebral aneurysms: the Duke Cerebrovascular Center experience in 235 patients with 274 stents. Neurosurgery 69:369-375, 2011
23. Lopes DK, Johnson AK, Kellogg RG, Heiferman DM, Keigher KM: Long-term radiographic results of stent-assisted embolization of cerebral aneurysms. Neurosurgery 74:286-291, 2014
24. Lubicz B, Francois O, Levivier M, Brotchi J, Balériaux D: Preliminary experience with the enterprise stent for endovascular treatment of complex intracranial aneurysms: potential advantages and limiting characteristics. Neurosurgery 62:1063-1069, 2008
25. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al.: Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke 41:110-115, 2010
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||