INTRODUCTION
A cerebrospinal fluid (CSF) shunt is the most common treatment known to date in the treatment of hydrocephalus. Several operational techniques were developed to divert CSF from the ventricular system to other spaces in the human body, such as the peritoneal cavity, the pleural cavity, and the right atrium, which also have CSF absorptive capabilities [10]. Among them, a ventriculoperitoneal (VP) shunt is one of the most commonly favored procedures for CSF diversion [12].
However, when the patient presents with abdominal CSF absorption abnormalities or infections, a VP shunt becomes unsuitable and an alternative site for CSF drainage is required. One alternative to VP shunting is ventriculoatrial (VA) shunting, but VA shunting is still rarely used as a first-line treatment due to cardio pulmonary and renal complications as well as surgeon’s preferences and bias [7]. We present a rare case where we first performed VP shunting and later changed to a VA shunt because of long-term abdominal distension.
CASE REPORT
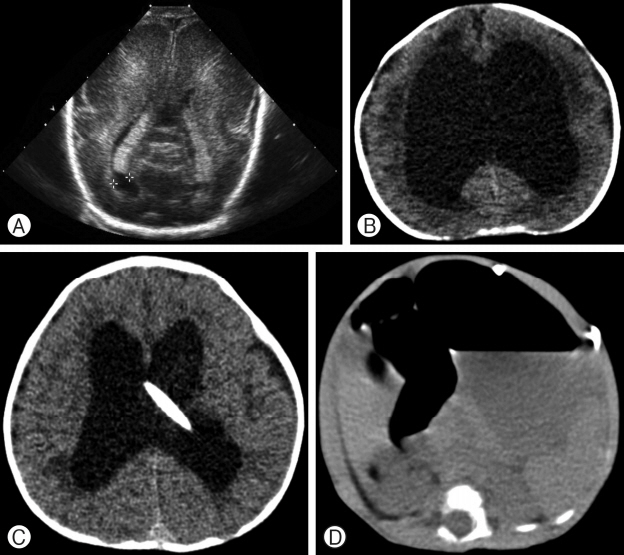
One of 2 twin girls, born 946 g at 26 weeks, was delivered by caesarean section. Brain ultrasonography was conducted immediately after birth and she was diagnosed with grade II germinal matrix hemorrhage with intraventricular hemorrhage (Fig. 1A). She also underwent an ileostomy surgery for neonatal necrotizing enterocolitis 10 days after birth. Post-hemorrhagic hydrocephalus was identified in the brain computed tomography (CT) scan, which was conducted around the 7th week after birth (Fig. 1B). Thereafter, she underwent several external ventricular drainage operations for post-hemorrhagic hydrocephalus and VP shunt surgery at 6 months of age (Fig. 1C). However, several months of vomiting and constipation ensued after the VP shunt surgery, and the abdominal distension worsened. At 8 months of age, a large amount of fluid collection within the peritoneal cavity was confirmed by an abdominal CT scan (Fig. 1D).
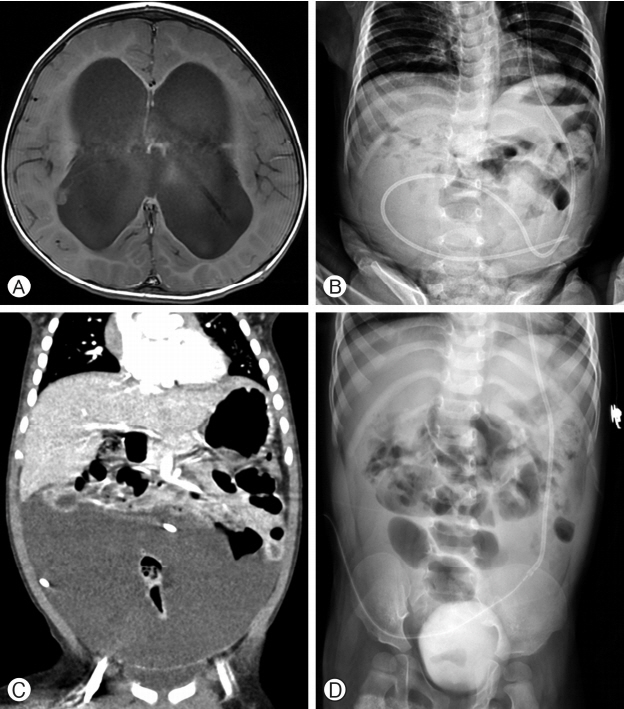
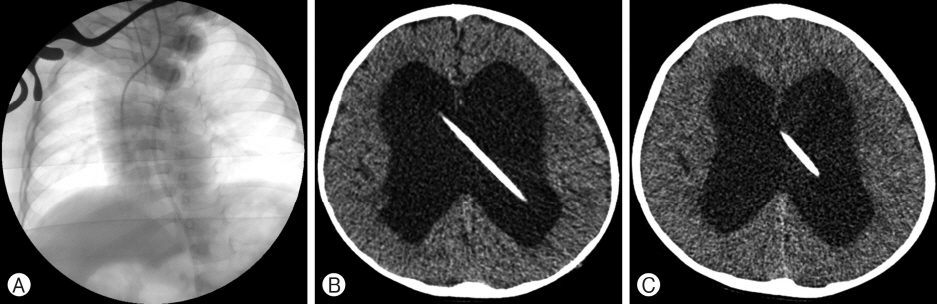
The patient was 11 months old when she first came to our hospital with a VP shunt for the moderately large lateral ventricles without choroid plexus hypertrophy seen on brain magnetic resonance imaging (MRI) (Fig. 2A). The abdominal distension continued, and ventricular dilatation progressed (Fig. 2B). CSF drained from the distal VP shunt catheter was poorly absorbed within the peritoneal cavity. At 27 months of age, the second abdominal CT scan again revealed a large amount of fluid collection within the peritoneal cavity (Fig. 2C). At 29 months of age, distal abdominal catheter externalization was temporarily performed (Fig. 2D). Twenty to 30 mL/kg of CSF per day was drained from 5 to 10 cm above the tragus point after distal abdominal catheter externalization, so CSF overproduction was suspected. Abdominal distension was still not resolved 2 weeks later even after the distal abdominal catheter externalization. VA shunting was performed with a Medtronic PS Medical, Inc. (Goleta, CA, USA) regular low pre- ssure valve. During insertion of the VA shunt, it was confirmed that the distal catheter tip was in the cavoatrial junction by intraoperative fluoroscopic imaging (Fig. 3A). The patient was discharged with improved abdominal distension and slightly smaller lateral ventricles (Fig. 3B). She was followed up for 3 years without any complications (Fig. 3C).
DISCUSSION
A CSF shunt is one of the standard treatments for hydrocephalus and is required for 12% to 14% of patients with severe post-hemorrhagic hydrocephalus [1,2,5]. Treatment methods for hydrocephalus aside from VP shunting include VA shunting, third ventriculostomy, choroid plexotomy, and choroidal artery embolization [6,13]. Although CSF shunt placement is the most com- mon procedure performed by pediatric neurosurgeons, shunts remain among the most failure-prone implantation devices in modern medical practice, with failure rates of 30% to 40% at 1 year and approximately 50% at 2 years in pediatric patients [3].
The most classical method of treatment for patients with hydrocephalus is the placement of a VP shunt where a distal catheter is placed into the peritoneal space, and it is important to recognize that intra-abdominal pressure can be one of the major determinants of effective shunt function. In such patients, constipation can result in significantly elevated intra-abdominal pressure that decreases CSF outflow through a distal catheter, resulting in shunt failure [9]. Surgery due to abdominal problems such as necrotizing enterocolitis can decrease intra-abdominal absorption and result in shunt malfunction [11]. In addition, abdominal distension from overproduction of CSF from choroid plexus hypertrophy has also been reported to affect shunt function [6].
VA shunts channel CSF from the ventricle of the brain into the right atrium of the heart. Although it is rarely considered as a first-line treatment because of cardiopulmonary and renal complications, VA shunting is a valid alternative in patients who have experienced multiple previous intra-abdominal VP shunt failures or had contraindications to abdominal catheter placement [14]. Recently, there are some reports that show no significant differences in mortality between patients with VP shunts and VA shunts, so in circumstances where it is difficult to perform a VP shunt, a VA shunt may be considered as an alternative [11].
When an intra-abdominal infection or abdominal surgery leads to an absolute decrease in CSF absorption, or when abdominal CSF absorption decreases due to absolute CSF overproduction especially due to choroid plexus hypertrophy, there is a high risk of VP shunt failure. In these cases, VA shunts should be considered rather than VP shunts [6,8]. Despite this, when CSF absorption is absolutely or relatively decreased in the abdominal cavity, the current opinion is that VA shunts should be recommended only after experiencing repeated VP shunt failures since VA shunts may yield serious complications [3,4,10].
However, it is the opinion of the authors of this investigation that in patients who demonstrate both CSF overproduction and a decrease in CSF absorption, a VA shunt should be strongly considered over a VP shunt. In particular, this may be especially applicable for patients who experience long-term abdominal distension from VP shunt failure when repeated VP shunts are highly likely to fail. Therefore, prompt VA shunts should be provided as the first-line treatment modality.
CONCLUSION
Although VA shunting is not routinely performed as the first-line treatment method due to many serious complications, it may be an alternative treatment modality if the VP shunt procedure is unable to be sustained due to multiple causes, such as long-term abdominal distension from CSF overproduc- tion and poor absorption.