INTRODUCTION
The common peroneal nerve (CPN) is crucial in maintaining a normal walking gait, and there are clinical situations where it is necessary to differentiate whether gait disturbance is caused by the central nervous system or spinal nerves6,18,38). In addition, the CPN is known as the most commonly injured peripheral nerve in the lower extremities due to its anatomical course7,8,35,37). In this review, we aim to describe the basic anatomy and function of the CPN and the common peroneal neuropathy (CPNe) caused by postures that are often encountered in the field of neurosurgery for the education of trainees, physician assistants, and neurosurgical fellows. In addition, diagnostic methods and treatments of the CPNe are reviewed including recently updated information that has not been included in previous reviews.
ANATOMY
The CPN is a branch from the sciatic nerve and descends obliquely along the lateral side of the popliteal fossa to the head of the fibula, coming close to the medial margin of the biceps femoris muscle and lying between the tendon of the biceps femoris and lateral head of the gastrocnemius muscle1,9-12,21,25,26,30,34). The nerve can be palpated behind the head of the fibula and as it winds around the neck of the fibula. On the basis of the magnetic resonance imaging (MRI) findings, the CPN is known to descend obliquely along the lateral side of the popliteal fossa, posterior to the short head of the biceps femoris muscle, and then lateral and superficial to the lateral head of the gastrocnemius muscle10,12,26). More inferiorly, it winds around the neck of the fibula (along the fibular tunnel), then enters the anterior and lateral muscle compartments of the leg and divides into the superficial and deep peroneal nerves. At this point, the nerve enters a tunnel formed by the two heads of the peroneus longus. The posterior edge of the peroneus longus, under which the nerve passes, can be thick and fibrous, acting as a constriction point between this and the lateral edge of the fibula18,19,35). Prior to passing through the fibular tunnel, the CPN gives off a branch called the lateral sural cutaneous nerve which provides sensory innervation on the posterior and lateral surface of the lower leg12) (Fig. 1).
Structures of the Fibula Tunnel
Humphreys et al.16) consider this tendinous leading edge the posterior crural intermuscular septum. In addition to this septum at the leading edge of the CPN, the deep tendinous fascia of the soleus muscle is present. After passing the leading edge of the peroneus longus, the next potential site of entrapment corresponds to the fascial septum between the peroneal and tibial anterior muscles known as the anterior crural intermuscular septum. As this nerve continues distally in the lateral compartment of the leg, it becomes superficial and pierces the crural fascia to become the dorsal cutaneous nerve at the distal third of the leg. Similarly, the deep peroneal nerve immediately gives off branches to the tibialis anterior after passing the fibrous edge of the peroneus longus. These branches keep the proximal aspect of this nerve branch tightly tethered in its position under the peroneus longus, as does its trajectory through the anterior intermuscular septum. This branch then continues distally in the anterior compartment of the leg, innervating the extensor hallucis longus, followed by the extensor digitorum longus and the peroneus tertius. Additionally, there is an unnamed distal intermuscular septum between the tibialis anterior and extensor digitorum longus muscles9,11,12,23,30). Although this is the most common anatomical orientation, numerous variations also exist. Nevertheless, neurosurgeons should know the above-described structures of the fibular tunnel, including four muscles, three septums, and one fascia (Fig. 2).
FUNCTION: MOTOR AND SENSORY
In Table 1, we describe the function of motor and sensory of the peroneal nerve. The boundary of the lower leg related to the CPN is divided by lateral and anterior compartments. The superficial peroneal nerve runs into and supplies the muscles of the lateral compartment of the leg for ankle eversion12). In addition, it supplies sensory innervation for the skin over the lateral lower two-thirds of the leg and the whole of the dorsum of the foot, except for the area between the 1st and 2nd toes, which is supplied by the deep peroneal nerve1,4,12,26,31,38). The deep peroneal nerve runs with the anterior tibial vessels over the interosseous membrane into the anterior compartment of the leg and then over the ankle to the dorsum of the foot. It supplies all of the muscles of the anterior compartment for dorsiflexion of the toe and ankle as well as providing a cutaneous supply to the area between the 1st and 2nd toes24,28,30,35,37).
CPN INJURY: MECHANISM OF PERIPHERAL NERVE INJURY
The CPN is susceptible to injury due to its superficial location, as it passes subcutaneously over the fibular neck and is the most commonly injured peripheral nerve of the lower extremity. In its limited location upon the hard surface of the fibula, it is particularly susceptible to direct trauma or laceration. In the textbook of “Youmans and Winn neurological surgery,” two major mechanisms of peripheral nerve injury are described according to energy force (high energy and lower energy)36) (Table 2). High energy injuries include avulsion, transection, stretch or contusion to the CPN combined with external wounds. In these cases, the neuroma-in-continuity (NIC) usually does not take place, and the subsequently injured nerve does not regenerate to and return to normal strength. The NIC results in a bump consisting of normal or abnormal healing structures of the injured nerve. Since patients with high energy injuries often visit the emergency clinic or orthopedic surgeons to intervene promptly, they are relatively rare in the neurosurgery field. Conversely, low energy injury includes entrapment, compartmentalization, and complex damage to the CPN; this results in low damage and regeneration to normal condition and without the immediate need for surgery7,10,28,35,36). Following, diagnosis and management is described focusing on patients with lower energy injuries, which are more commonly encountered in neurosurgery.
DIAGNOSIS
1. Physical Examination
Patient history and neurological examination are the most important initial clinical approaches for reaching a diagnosis of suspected peroneal neuropathy. Although an accurate misdiagnosis rate has not been reported, Baima has reported that ankle inversion by the tibialis posterior muscle showed ankle dorsiflexion, making it difficult to discriminate from dropped foot caused by peroneal nerve palsy4,22,37,38). There are several clinical pitfalls that make differentiation from discogenic foot drop difficult. First, the situation of patients that had experienced back pain and paresthesia of the affected lower extremity in the past and had been treated for the herniated lumbar disc, now visiting the hospital once again due to worsened herniated lumbar disc symptoms may limit clinicians in having adequate time for thorough enough history taking to make an accurate diagnosis, leading to inappropriate evaluations and unnecessary treatments. Second, as referred pain by CPN can be felt from the knee and the lateral thigh to the dorsum of the foot, patients may describe referred pain as radiculopathy following from the above, complaining of paresthesia and sensory deficit. Clinicians accustomed to referred pain related to discogenic radiculopathy can mistake the symptoms for the herniated lumbar disc. Third, in some clinical aspects, complete palsy of CPN caused by direct injury can be mistaken for foot drop, as it is not always accompanied by sensory disturbance and can easily be misdiagnosed. As the gluteus muscle is mostly innervated by the lumbosacral plexus, assessment of hip abductor muscle strength in foot drop patients is useful in differentiating CPN palsy from lumbar radiculopathy, with 85.7% sensitivity and 96.4% specificity17). The author also believes that as ankle-foot motion is variable or patients are not accustomed to specific ankle motions, such as ankle inversion or eversion, it is useful to evaluate the strength of muscles that CPN does not innervate. A diminished hip abductor muscle tone can also be simultaneously observed in patients with a lumbar disc herniation that may induce a foot drop. A similar method tests non-evoked pain in the straight leg raise test of the affected leg, meaning the possibility of discogenic foot drop is low. Therefore, patients with CPN palsy always complain about sudden-onset ankle dropping, which is more severe than in cases of a herniated lumbar disc, and are not bothered by sensory disturbance or pain.
2. Electrodiagnostic Study (EDX)
In most cases of peroneal nerve palsy induced by posture, the nerve injury type is neuropraxia according to the Seddon classification system. Hence, although a peroneal motor nerve conduction study should be performed first, recording from the extensor digitorum brevis muscle with a superficial peroneal sensory nerve action potential (SNAP) is important to help differentiate from L5 radiculopathy. An abnormality in SNAP implies that the lesion is distal to the dorsal root ganglion. However, it is rare to reveal pure CPNe with certainty on the EDX, and it is often reported along with radiculopathy due to a herniated lumbar disc. Because of this ambiguity, neurosurgeons may suspect CPNe after physical examination and should be able to read the EDX with a focus on denervated muscles innervated by the peroneal nerve. In Table 3, it may be reported as lumboradiculopathy combined with or without CPNe. In this case, acute fibrillation and a positive sharp wave of the tibialis anterior, extensor hallucis longus, and peroneus longus may serve as the diagnostic evidence for the CPNe.
3. MRI
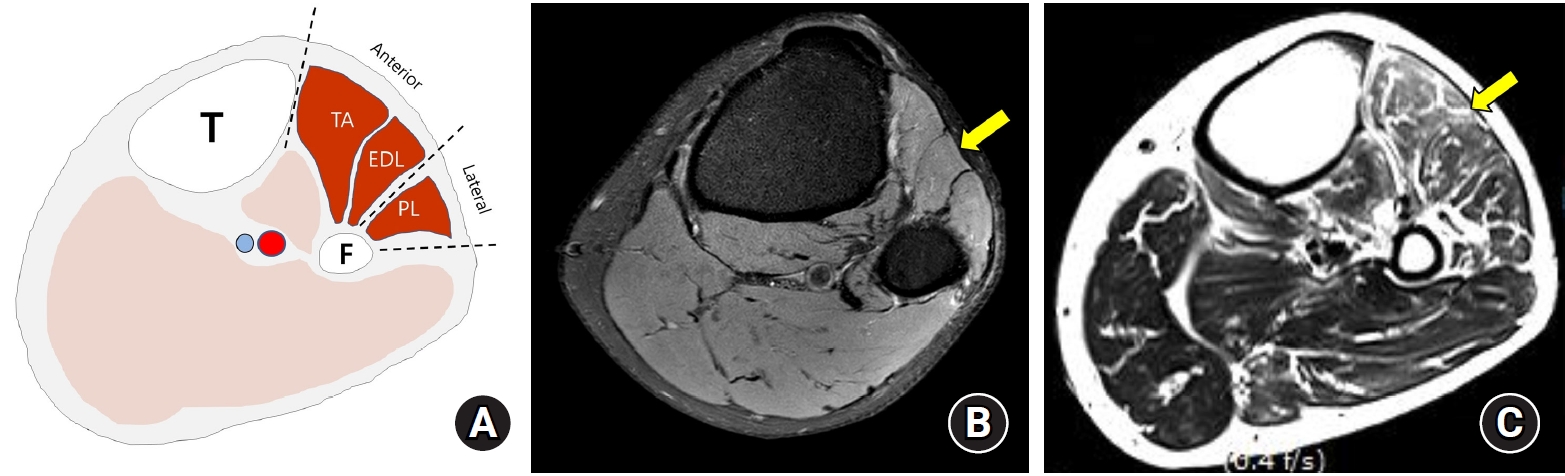
For EDX, patients must wait for Wallerian degeneration to begin after the onset of symptoms, and thus and it often takes considerable time to receive a diagnosis5,11,19,33). However, MRI requires no waiting time and plays an important role in the detection and characterization of pathologic conditions of skeletal muscles that cause changes in muscle signal intensity. The CPN innervates the muscles of the anterior and lateral compartments of the lower leg. For this reason, using conventional MRI, CPNe may be diagnosed with signal changes of denervated muscles, i.e., the peroneus longus in the lateral compartment, and the extensor digitorum longus and the tibialis anterior in the anterior compartment8) (Fig. 3A).
Muscle denervation results in enlargement of the intramuscular capillary bed, causing an increase in the muscle blood volume8,11,19,33). In addition, there is an increase in extracellular fluid within the denervated muscles. The latter is likely a result of the increased muscle cell membrane permeability and reduced Na-K-ATPase function seen in denervated muscle. These events are thought to contribute to the T2 signal abnormality seen in the denervated muscles on MRI, though it is not clear whether this results from a combination or any one of these factors alone. Peripheral nerve injury also produces morphologic and metabolic changes in the denervated muscles, and glucose uptake in muscle fibre decreases while glycolysis increases. Furthermore, denervation induces proteolysis in the skeletal muscle. These metabolic changes occur soon after nerve damage and are manifested histologically by reducing muscle fibre diameter in the denervated muscle. With atrophy of the muscle fibres there is a relative increase in their fat content compared with protein content, and chronic denervation results in diffuse fatty infiltration of the affected muscle with associated loss of muscle bulk. In experimental studies, the first non-specific histological changes are seen approximately 10 to 12 days after denervation in the form of moderate atrophy of the muscle fibres. The typical histological findings of denervation, however, tend to appear 3 weeks after the initial event. Several clinical and experimental studies have demonstrated signal changes in denervated muscles on MRI, and experimental animal studies have demonstrated changes as early as within 24 hr. In clinical studies, abnormal signal intensity within the denervated muscles has been demonstrated within 4 days of injury. Short Tau Inversion Recovery images are highly water-sensitive, with the timing of the pulse sequence acting to suppress signals from fatty tissues, so water is highlighted on the image. The acutely and subacutely denervated muscle shows a high signal intensity pattern on fluid sensitive sequences and normal signal intensity on T1-weighted MRI images. In chronic denervation, muscle atrophy and fatty infiltration demonstrate high signal changes on T1-weighted sequences associated with volume loss (Table 4, Fig. 3B, C)8).
TREATMENT AND OUTCOME
Generally, medications without surgical intervention are the primary treatment method for CPN injury, since most patients experience spontaneous recovery within 2 to 3 months. However, not all patients experience clinical improvements spontaneously, and some have permanent walking disabilities. In practice, posture-induced CPN palsy patients tend to undergo passive treatments and increased waiting times due to a benign prognosis by clinicians2,22,23,36,38).
1. Non-operative Management6,22,23,27,38)
In patients with acute painful neuropathy (usually not presenting), first-line simple analgesics such as non-steroidal anti-inflammatory drugs and acetaminophen may decrease symptoms. With intractable or chronic neuropathy, anti-seizure medications such as gabapentin and pregabalin may relieve sensory disturbances such as paresthesia, anesthesia, and algesia. In one recent study, Vitamins B-1, B-6, and B-12 have been found to be especially beneficial for treating neuropathy. Specifically, vitamin B-1, also known as thiamine, has been shown to help reduce pain and inflammation, and vitamin B-6 preserves the covering of nerve endings. Aside from medications, ankle and foot braces (ankle-foot orthosis [AFO]) that fits into the patient’s shoe may hold the ankle in a normal position preventing gastrocnemius shortening or contracture until the restoration of motor function is complete. Strengthening of the tibialis anterior muscle and stretching of the gastrocnemius muscle also help maintain the range of motion in knee and ankle and may improve gait disturbance related to dropped foot. This combination of medication, AFO, and physiotherapy does not apply to all patients with CPNe, and should always be considered depending on clinical presentation.
2. Operative Management
1) External neurolysis and decompression13,16,20,32,35)
Surgical techniques to restore the function of the CPN exist; however, as mentioned previously, surgical methods are dependent on the etiology of the damage to the CPN and the time period elapsed since injury. In cases of high-energy injury such as fracture, contusion, laceration, and stretch, direct repair or exploration within 3 weeks is recommended. Conversely, if dropped foot is caused by low-energy injury such as certain prolonged posture (habitual leg crossing, squatting, and sleeping), neuropraxia of the CPN as determined by the Seddon classification system (equal to Grade 1 of Sunderland classification system) is the most common. In most cases, the patient will return to normal function without surgical treatment; however, in some cases where spontaneous recovery does not occur for more than 2 to 3 months, neurolysis should be considered. At this point, the CPNe is considered to be accompanied by an alteration of anatomical structures at the level of the fibular tunnel, and the purpose of surgery is to maximize the regeneration potential of the CPN by external neurolysis between the CPN and the structures of the fibular tunnel as described above.
Surgical technique16)
For this procedure, patients are placed under general anesthesia and positioned supine with the knees of the affected side flexed at a 60-degree angle. CPN is palpated if possible, and if not, sonography is utilized preoperatively to locate it precisely. A curved incision just below the lateral aspect of the head of the fibula is made. Subcutaneous tissues are dissected to expose the CPN, which is then explored distally to determine the sites of compression that originally caused neuropathy. Hypertrophy of deep tendinous fascia, anterior and posterior crural intermuscular septum, and intermuscular septum are carefully examined. The development of adhesion tissues around the course of the CPN is investigated as well. After choosing the appropriate target for decompression among the aforementioned structures, external neurolysis is performed using resection of thickened septum and fascia. If the extent of decompression is deemed appropriate, an anti-adhesion barrier agent is applied in the operative field. Finally, the surgical wound is closed layer-by-layer.
Surgical outcome16,20,27,35)
In 2013, Doctor Maalla and his colleague20) from Tunisia studied “Peroneal nerve entrapment at the fibular head: Outcomes of neurolysis. They retrospectively reviewed the medical charts of 15 patients (mean age, 32 years) treated with neurolysis. The diagnosis was idiopathic CPN entrapment in ten patients, indirect nerve injury with CPN paralysis due to an ankle injury in three patients, and postural CPN compression in two patients. The mean time to management was 7 months (range, 2-18 months). The authors concluded that spontaneous recovery could take time and remain incomplete and preferred to perform surgery between the third and fourth months in patients with persistent symptoms or incomplete recovery, even in forms confined to sensory dysfunction documented by electrophysiological testing. Time to recovery is shorter after surgical decompression than with rehabilitation therapy. Moreover, Humphreys et al.16) reported good results of decompression of the CPN and performed this operation frequently. Postoperatively, 40 (83%) of 48 patients who had preoperative motor weakness improved motor function. Likewise, 23 (49%) of 47 patients who had sensory disturbances and 26 (84%) of 31 patients who had preoperative pain improved after surgical decompression of the peroneal nerve.
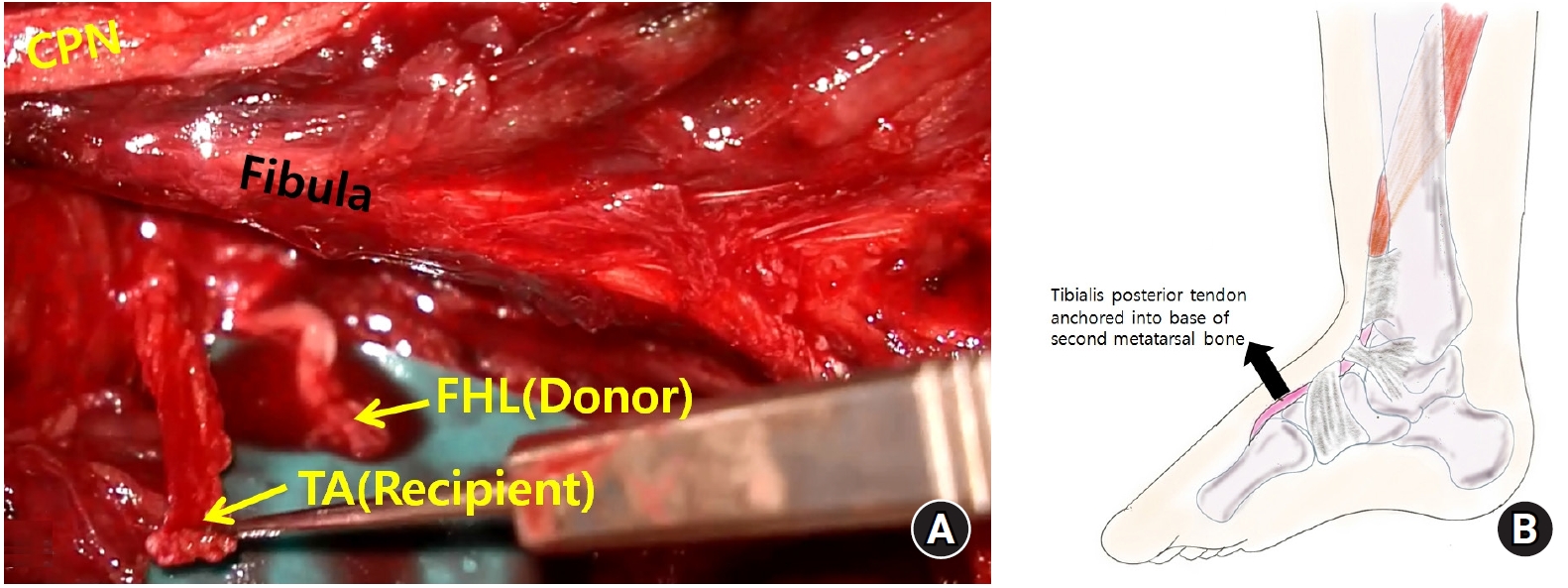
2) Nerve transfer and tendon transfer
Among the muscles controlled by the CPN in normal walking, the function of the tibialis anterior muscle is the most important. Therefore, nerve transfer and tendon transfer should be considered for patients who are unable to walk normally because dropped foot has not recovered despite active treatment including neurolysis (Fig. 4A, B). The purpose of both surgeries is to restore function of tibialis anterior muscle, and in the case of nerve transfer, a motor branch in an adjacent area with normal function is used as a donor nerve, and a motor branch that controls tibialis anterior muscle becomes the recipient and connect it. Common donor nerves are motor branches of flexor hallucis longus and lateral gastrocnemius14,15). Moreover, there is a tendon transfer that moves posterior tibia tendon to the dorsum of the foot to keep the ankle in a neutral position. In the case of these two surgical methods, wearing an AFO and rehabilitation are both mandatory. If muscle atrophy has progressed due to long-term denervation, nerve transfer cannot be performed and posterior tibial tendon transfer is required3,29).
CONCLUSION
Dropped foot is a troubling symptom that makes daily life inconvenient with difficulty and instability in walking. Patients with dropped foot due to CPNe can often be encountered in neurosurgery departments, and it is important to accurately diagnose them and be able to explain the treatment and prognosis. Therefore, it is mandatory to be aware of the course of this nerve and its structure at the level of fibular tunnel. Physical examination and history-taking are essential for diagnosis, and in addition to the EDX, it is possible to diagnose the CPNe using the MRI appearance of denervated muscles. If neurosurgeons become familiar with the anatomy of the CPN, neurolysis can be easily applied and may lead to a good prognosis for patients with CPNe.