Salmonella Typhimurium Brain Abscess in an Immunocompetent Adult with a Spontaneous Intracerebral Hemorrhage: A Case Report
Article information
Abstract
A brain abscess caused by Salmonella typhimurium (S. typhimurium) in an immunocompetent adult is rare. We report a case of brain abscess caused by S. typhimurium in a 46-year-old male and a brief review of the literature. The patient visited a local hospital because of right hemiparesis. Brain computed tomography and magnetic resonance imaging results showed an acute hematoma in the left basal ganglia. After 3 weeks of conservative therapy, the patient was transferred to our hospital due to uncontrolled fever, aphasia, and aggravated motor weakness. Contrast-enhanced computed tomography showed a rim-enhanced cystic mass with peripheral edema, prompting trephination to drain the cystic fluid. The drained fluid was yellowish-mucoid, similar to a pus. Specimens from the drained fluid and urine S. typhimurium were cultured and microbiologically analyzed. We administered ceftazidime 2,000mg and vancomycin 2,000mg/day for 6 weeks intravenously and changed ceftriaxone 2,000 mg/day for an additional 3 weeks due to a drug eruption. The patient recovered with no neurological deficits. Surgical drainage of the intracranial abscess and prolonged sensitive antibiotic therapy is essential to obtain positive results.
INTRODUCTION
Although Salmonella species can cause focal subdural or epidural empyema and brain abscesses in any age group, most reported cases are patients with precipitating factors, such as immunocompromised conditions (e.g., human immunodeficiency virus [HIV] infection, chemotherapy, long-term steroid therapy), blood problems (e.g., sickle cell disease), previous brain surgery or infarcted brain tissue, hepatic or gastrointestinal disease, alcohol abuse, or infancy1,3,5,7,8,11,13,15). Intracerebral infections caused by Salmonella are rare. Here, we present a rare case of an intraparenchymal brain abscess caused by Salmonella typhimurium (S. typhimurium) at the site of a liquefied intracerebral hemorrhage (ICH).
CASE REPORT
A 46-year-old man visited a local hospital because of right-sided weakness. On neurological examination, the patient showed right hemiparesis and mild dysarthria. Brain computed tomography (CT) and magnetic resonance imaging (MRI) showed acute ICH in the left basal ganglia (Fig. 1). The patient was treated with mannitol alone, and his neurological symptoms were not aggravated. On the 23rd day of admission, the patient suffered from malaise and a severe headache. On the 25th day, he was referred to our hospital because of uncontrolled fever, aggravated hemiparesis, and motor aphasia. A follow-up enhanced brain CT scan revealed a rim-enhancing hypodense lesion and massive peri-lesional edema (Fig. 2A). We performed an emergency trephination to drain the cystic mass lesion in the left basal ganglia. The drained fluid was not a chronic liquefied hematoma; instead, it was yellowish-mucoid in nature and gave a characteristic odor when it was an abscess. After the operation, we rechecked the brain MRI and suspected an intracerebral abscess (Fig. 2B, C). The patient had been healthy prior to the occurrence of spontaneous ICH. He did not have gastrointestinal symptoms, meningeal signs, or immunocompromised indications. The results of the blood examination were white blood cell (WBC) 14,300/μL, C-reactive protein (CRP) 72.98 mg/L, erythrocyte sedimentation rate (ESR) 73 mm/hr, hemoglobin 13.4 g/dL, platelets 164,000/μL, and HIV Ab (−). Evaluation of the cerebrospinal fluid revealed the following values: WBCs, 2/mm3 with 0% neutrophils and 0% lymphocytes, red blood cells, 71/mm3, glucose, 75 mg/dL, protein, 31.1 mg/dL, and no growth on culture.
Brain computed tomography (CT) and magnetic resonance imaging (MRI) from a local hospital. The brain CT showed a hyperdense lesion on the left basal ganglia (A), and a MRI scan (T2-weighted, diffusion-weighted, axial section) showed hypointensity in the same area (B, C) consistent with an acute hematoma.
Enhanced brain computed tomography (CT) and magnetic resonance imaging (MRI) at our hospital. A rim-enhancing hypodense lesion and perilesional edema were found on enhanced CT (A). The postoperative MRI diffusion-weighted image showed a hyperintense lesion (B) and T1 enhanced image showed ring-enhanced lesion (C) in the same area, suspicious for a brain abscess.
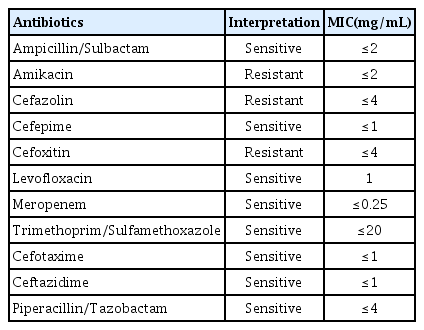
On microbiological analysis, S. typhimurium was cultured from the pus and urine (Fig. 3). In the blood culture, there was no growth of bacteria. Microbes were identified as Salmonella group using the Vitek 2 XL system (bioMérieux, Nürtingen, Germany), and the serotype was identified as S. typhimurium using Salmonella antisera (JoongKyeom, Ansan, Korea). We administered ceftazidime 2,000 mg and vancomycin 2,000 mg/day for 6 weeks via an intravenous route based on the antimicrobial susceptibility test (Table 1) and changed ceftriaxone 2,000 mg/day for an additional 3 weeks due to the occurrence of a drug eruption caused by vancomycin.
Round, gray colonies on a 5% sheep blood agar plate (A), and colorless colonies on a MacConkey agar plate (B) were observed at 24 hr incubation at 37°C, 5% CO2 conditions. It produced hydrogen sulfide on a Salmonella-Shigella Agar plate (C) and showed a red slant/yellow bottom (alkali/acid reaction) with hydrogen sulfide in triple sugar iron agar (D). Gram-negative bacilli from a blood agar plate (Gram stain, ×1,000 magnification) (E).
The patient recovered normal neurological status, and follow-up ESR/CRP conducted at week 9 of hospitalization was normalized (Fig. 4). Follow-up at one year after MRI showed only focal encephalomalacia in the left basal ganglia and temporal area (Fig. 5).
DISCUSSION
Intracranial infections (meningitis, subdural or epidural empyema, brain abscess) caused by Salmonella species are very rare. Since the first Salmonella brain abscess was reported by McClintock in an autopsy study in 1902, fewer than 100 cases of intracranial Salmonella infections have been reported 18,19,22). Among intracranial infections, brain abscesses remain the rarest, and, to our knowledge, only 12 cases of brain abscess caused by S. typhimurium have been reported (Table 2)3,6,7,10–13,16,19,21,23). However, intracranial infections associated with Salmonella species have increased recently because of the number of immunocompromised patients with acquired immunodeficiency syndrome (AIDS), corticosteroid therapy, broad-spectrum antibiotic use, or chemotherapy has been increasing 13,22). Although intracranial Salmonella infections can occur at any age, they tend to be more common in infancy because of the immunologically naïve state13,16,19).
According to Mahapatra and Bhatia, infectious routes for brain abscesses caused by Salmonella can be divided into 3 groups17). First, patients develop a brain abscess during a Salmonella infection elsewhere in the body. Second, patients have a history of Salmonella infection. In the third group, patients presented with a brain abscess with no apparent history of salmonellosis. Our patient had no history of Salmonella infection. Although S. tiphymurium was cultured from his urine and drained pus, his blood culture was negative. The patient did not suffer from gastrointestinal symptoms and had no risk factors for decreased immunity.
Intracranial Salmonella infections tend to involve diseased tissues, such as hematomas, fractures, and neoplasms22). In our case, diseased tissue and liquefied hematoma may have acted as the culture medium. Systemic diseases including malaria, sickle cell anemia, diabetes mellitus, AIDS, systemic lupus erythematosus, hepatic disease, gastrointestinal disease, alcohol abuse, corticosteroid therapy, and chemotherapy are other factors associated with salmonellosis8,11,13). In addition, focal infections adjacent to the brain, such as otitis, paranasal sinus infection, meningitis, and osteomyelitis of the skull, are other precipitating factors22). In the previous literature on S. typhimurium brain abscesses, 3 cases presented with focal infections adjacent to the brain, 4 cases were in infants, 2 cases were in AIDS patients, one case involved alcoholism, 1 case had a previous stroke history, and the present case involved a previous ICH site (Table 2)3,6,7,10–13,16,19,21,23).
Several factors contribute to the pathogenesis of salmonellosis: the Salmonella inoculum size, the virulence of the strain, the host immune response, and local protective factors22). Thus, Salmonella infection in humans shows a spectrum of symptoms from asymptomatic carriers to focal localized infections, such as meningitis, brain abscess, gastroenteritis, or cholecystitis, and sometimes even bacteremia8,22). Likewise, the clinical presentations of Salmonella brain abscesses vary from simple headache or vomiting to altered states of consciousness or focal neurologic deficits.
Salmonella is a facultative intracellular organism, and a cell-mediated immune response depends on macrophage function 2,9,24). Increased susceptibility to Salmonella infection is thought to be due to several factors: prolonged exposure to the organism, impairment of the cell-mediated immune response, impairment of phagocytosis, alterations in local protective factors, and the presence of diseased tissue4,8,25).
Determining the location and size of an abscess through CT and/or MRI and identifying the organism involved in pus culture is crucial for an accurate diagnosis and adequate treatment of brain abscess caused by Salmonella. Such abscess could be treated through surgical drainage and combined antibiotic therapy1,13,22). In our review, almost all patients who died from brain abscesses caused by S. typhimurium did not undergo surgical drainage (Table 2). Chloramphenicol, a third-generation cephalosporin, and trimethoprim/sulfamethoxazole are the drugs of choice after pus drainage. Salmonella strains resistant to these antibiotics are uncommon14,22). In addition, long-term antibiotic therapy—at least 6 weeks—is essential because of the risk of recurrence. In our case, we administered ceftazidime, based on culture sensitivity, and vancomycin to prevent scalp and tract infections.
CONCLUSION
We report a rare case of an intracranial abscess caused by S. typhimurium at a previous spontaneous ICH site. Surgical drainage of the intracranial abscess and prolonged sensitive antibiotic therapy are essential to obtain positive results. In particular, we emphasize that early surgical drainage reduces mortality, as it prevents the unnecessary use of broad-spectrum antibiotics through pus culture.
Notes
No potential conflict of interest relevant to this article was reported.