Simultaneous Cranioplasty vs. Staged Cranioplasty for Reconstruction of Bilateral Craniectomy
Article information
Abstract
Objective
Cranioplasty (CP) following decompressive craniectomy (DC) is of low complexity surgically. However, even this “simple” procedure may have a high complication rate, especially for the reconstruction of bilateral craniectomy compared to the reconstruction of unilateral craniectomy. This study aimed to assess and compare the rate of complications between simultaneous and staged CP for the reconstruction of bilateral craniectomy.
Methods
All patients who underwent CP at our institution following DC for stroke or traumatic brain injury between 2008 and 2017 were reviewed. A total of 139 patients were identified, of whom 17 underwent bilateral CP. Simultaneous and staged CP was performed in 6 and 11 patients, respectively. The median time from craniectomy until CP was 94 days (range, 25-220 days). In patients with staged CP, the interval between the first CP and the second CP was 15 days (range, 6-43 days). The overall rate of complications, such as postoperative bleeding, seizures, postoperative infection, and hydrocephalus, was 16%.
Results
There were no statistically significant differences in outcome variables between simultaneous CP and staged CP for the reconstruction of bilateral craniectomy, except for estimated blood loss. The estimated blood loss was lower in patients who underwent staged CP than in those who underwent simultaneous CP. The length of hospital stay was naturally longer when staged CP was performed.
Conclusion
No significant differences were found in outcome variables between simultaneous and staged CP for the reconstruction of bilateral craniectomy, except for estimated blood loss and the length of hospital stay. Therefore, simultaneous CP might be more beneficial for economic reasons than staged CP.
INTRODUCTION
Decompressive craniectomy (DC) is a crucial procedure for elevated intracranial pressure refractory to medical treatment followed by traumatic brain injury, intracranial hemorrhage, brain infarction, and so on5,14,21,24). Skull defect following DC can be restored by performing cranioplasty (CP)1,3,6,8,10,11). CP has multiple positive effects such as improving cerebral hemodynamics, restoring outward appearance, enhancing protection, reducing epileptic seizures, and helping patient’s rehabilitation8,10,11,15,20,22,23,25,28). CP is a relatively simple neurosurgical procedure with many benefits. However, when, how, and by what it is performed can make many differences1,2,4,7,14,16,19,20,23,27-29).
Although CP has many benefits, CP also has many side effects like blood loss, increased hospital stay, infection, the risk of hydrocephalus, and the possibility of developing “trephined” syndrome1,3,9,13,17,26,29). Although the mortality rate after CP is low, complications occur more than expected12,29).
Matters of when, how, and by what CP is performed has been discussed in many studies. For some reason, bilateral CP is performed at the same time or the initial DC and sequentially after the initial DC by time. The objective of this retrospective study was to determine whether bilateral CP performed after the initial DC might be better than bilateral CP done simultaneously with the initial DC.
MATERIALS AND METHODS
This retrospective study was reviewed and approved by the Ethics Committee (IRB No. 2022-0661-0001).
1. Patient Population
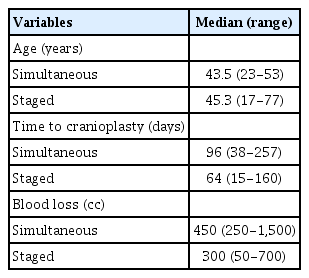
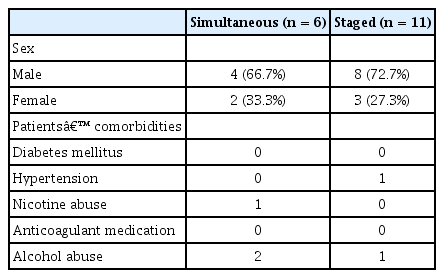
The 139 patients who underwent CP from 2008 to 2017 were analyzed. Of them, 17 met the inclusion criteria. Inclusion criteria were: bilateral CPs were done less than six months after initial DC; all staged CPs were done less than one month in the interval; all CPs were done using autologous bone; and all DCs were done after traumatic brain injuries. These inclusion criteria were used to minimize the bias of analysis. All operations were performed by two skillful brain surgeons. Demographic characteristics and other variables are summarized in Tables 1 to 3 and Fig. 1. For bilateral CPs, six were done simultaneously (simultaneous group) and 11 were done by time (staged group). The mean age of patients was 43.5 years (range, 23-53 years) for the simultaneous group and 45.3 years (range, 17-77 years) for the staged group.
2. Cranioplasty
All CPs were done in a standard fashion. Incisions were made following the incision of the previous operation. The scalp and muscle flap was reflected to reveal the defect. Coagulation was done by the sight of active bleeding. If any tissues were present at the edge or over the defect, they were removed and cleaned. Autologous bone was placed and fixed to the skull with a titanium plate and screws. Several small holes were made by drilling into the bone to prevent accumulation of any fluid. Muscles and scalp were then sutured in a counter fashion after applying subgaleal drains. When bilateral DC was done, every flap was made using a bi-frontal double flap instead of a bi-coronal flap. For every patient, subgaleal drains were applied and left for 1 to 3 days. Autologous bone was used for every patient. It was stored at -80°C in the fridge immediately after DC. Prophylactic antibiotics were used for one day.
3. Statistical Analysis
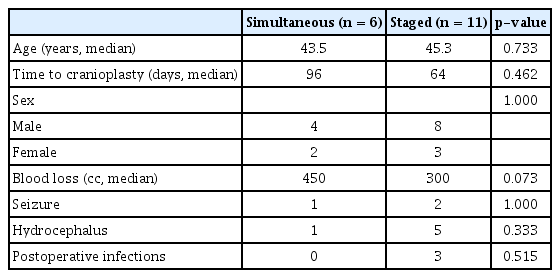
All statistical analyses were conducted using SPSS statistics version 27 (IBM Corp., Armonk, NY, USA). Most analyses in this study were done using a non-parametric test. Demographic characteristics, patient comorbidities, and blood loss during operation were analyzed using the Mann-Whitney U test. Complications such as seizure, hydrocephalus, and postoperative infection were analyzed using Pearson’s χ2 test and Fisher’s exact test. Duration of hospital stay was analyzed with an independent t-test which was a parametric statistics technique. A significance threshold of p < 0.1 was used throughout.
RESULTS
Within 10 years of the study period, 139 patients had DC followed by CP. A total of 17 patients who underwent bilateral DC and bilateral CP were included in this study. Only those who had DC after traumatic brain injury were included to reduce bias. Six out of 17 patients had bilateral CP simultaneously and 11 had bilateral CP done by time (staged CP). All CPs were done less than 6 months after the initial DC. All staged CPs were done with an interval of less than one month.
Complications and Hospital Stay
Regarding complications, seizure, hydrocephalus within three months, infection after surgery, and blood loss during surgery were analyzed. In order of their frequency, hydrocephalus (n = 6 patients, 1 in simultaneous group/16.7%, 5 in staged group/45.5%), seizures (n = 3 patients, 1 in simultaneous group/16.7%, 2 in staged group/18.2%), and infection after surgery (n = 3 patients, 0 in simultaneous group/0%, 3 in staged group/27.3%) occurred (Table 3). Resorption occurred in two patients. However, it was not counted as a variable for analysis. Blood loss during surgery was obtained by searching operation record and double-checked with anesthesia record. Blood loss during staged cranioplasties was calculated by adding up both operational results. Blood loss during operation was statistically higher in the simultaneous group than in the staged group. There was no statistically significant difference in complications except for blood loss (Table 4). The duration of hospital stay was naturally longer when staged CP was done (Table 5).
DISCUSSION
Although CP is a simple procedure, it has a relatively high complication rate. Reducing complications and hospital stay can be beneficial for both patients and surgeons17-19,23,27,28). In some cases, bilateral craniectomies are done. However, bilateral craniectomies can have more complications than unilateral craniectomies. Bilateral craniectomies can be done simultaneously or sequentially after the initial DC. Due to the higher chance of complications of bilateral CP than unilateral CP, efforts are needed to reduce complications and improve outcomes. The aim of this retrospective study was to determine whether bilateral CP performed after the initial DC (staged one) might be better than bilateral CP done simultaneously with the initial DC (simultaneous one).
Whether doing it simultaneously or on time depends on many conditions. Surgeon’s preferences, patient’s condition, operation room capability, existence of prior postoperative infection, patient’s positioning during surgery, possibility of infection when changing position during operation, and so on should be considered when deciding when or how to perform bilateral CP.
Our data suggest that other than differences in blood loss and duration of hospital stay, there was no significant statistical difference between the two ways of CP. According to our data, simultaneous CP might be more beneficial for outcome and economic reasons than staged CP.
This is the only study on whether simultaneous CP is more beneficial than staged CP. However, our study had some limitations. We tried our best to reduce bias for better outcomes as much as we could by simplifying and unifying variables. In addition, every craniectomy was recruited due to a traumatic brain injury. Moreover, all cranioplasties were done using autologous bones. However, a such effort led to an insufficient number of targeted patients. Because of the small sample size, we had to use patients operated by two different surgeons. Thus, surgeon capability might be another bias. In addition, due to its retrospective and non-randomized nature, this study had a potential selection bias. Due to the small number of patients, statistics might lack reliability. Thus, further trials on a larger scale with multiple cases are needed in the future. If possible, multi-center or multiple doctor involvement is needed to analyze surgeon capability factors.
CONCLUSION
There were no significant differences in outcome variables between simultaneous and staged CP for the reconstruction of bilateral craniectomy except for estimated blood loss or duration of hospital stays. Performing bilateral CP at once can be beneficial for patients and surgeons.
Notes
No potential conflict of interest relevant to this article was reported.