The Influence of Spondylolisthesis Reduction on the Adjacent Lumbar Segment
Article information
Abstract
Objective
Mild to moderate stenosis at the adjacent level sometimes co-occurs with lumbar spondylolisthesis, but whether to include the adjacent level during surgery for the index level is a matter of debate. Spondylolisthesis causes anterior slipping of the vertebra and reduces the segmental angle (SA) at the index level, and the adjacent level may compensate for this change through hyperextension to maintain spinal balance. This study investigated the radiological changes and clinical outcomes of adjacent segment stenosis in patients with lumbar spondylolisthesis.
Methods
Forty consecutive patients (12 men and 28 women, age 66.6±10.4 years) underwent single-level oblique lumbar interbody fusion for L4-5 or L5-S1 spondylolisthesis. Lumbar central stenosis at the cranial adjacent segment was present in 16 patients (stenosis group) and absent in 24 patients (no-stenosis group). Clinical and radiological parameters were longitudinally compared between the stenosis and no-stenosis groups.
Results
Both groups showed similar and significant clinical improvement. The SA at the index level significantly improved in both groups (p<0.05), but the SA at the cranial adjacent segment significantly decreased only in the stenosis group (p<0.05). The spinal canal area at the adjacent level significantly improved only in the stenosis group (p<0.05).
Conclusion
Realigned spondylolisthesis may reduce hyperextension of the adjacent segment. If mild lumbar spinal stenosis is present at an adjacent level to spondylolisthesis, it may not be essential to include it in surgery.
INTRODUCTION
Lumbar spondylolisthesis is a common spinal degenerative disease that requires spinal fusion surgery when instability is also present5,31). Adjacent segment stenosis sometimes coexists with spondylolisthesis, but deciding how to address the adjacent segment stenosis is relatively complex8,23,28). Previous studies have analyzed the importance of adjacent segment disease (ASD) and showed progressive degeneration at adjacent segments after fusion surgery during follow-up7,8,32). Biomechanical studies have shown that the intradiscal pressure at the adjacent segment increased after instrumented fusion and spinal fusion surgery was a risk factor for adjacent segment degeneration28,30). Considering ASD during follow-up, pre-emptive simultaneous decompression surgery may be an attractive option2,16,23,28). However, asymptomatic stenosis may not be a poor prognostic factor, and decompression surgery may increase surgical costs, prolong the hospital stay, and enhance degenerative processes at the adjacent segment2,16,19,23,28). Spondylolisthesis causes anterior slipping of the vertebra and a decrease in the segmental angle (SA) at the index level, and the adjacent level may compensate for this change by hyperextension to maintain spinal balance12). Hyperextension may lead to buckling of the ligamentum flavum and consequent spinal stenosis.
The fused lumbar segment may increase stress on the adjacent segment28,30), but realigned spondylolisthesis may decrease hyperextension in the adjacent segment. Consequently, decreased hyperextension of the adjacent segment may reduce the concern for ASD. However, previous studies of ASD after fusion surgery did not separate patients with spondylolisthesis2,16,23,28). A recent study showed the benefit of minimally invasive fusion surgery for ASD, and the potential benefit of spinal realignment with minimally invasive fusion surgery may compensate for the disadvantage of altered biomechanics at the adjacent segment after fusion surgery15,18).
Most previous studies have reported radiological changes and their influence on clinical outcomes, but studies discussing hyperextension at the adjacent segment are scarce2,7,8,15,16,19,23,28,32). Although differentiating symptomatic and asymptomatic adjacent segment stenosis was difficult, we performed oblique lumbar interbody fusion (OLIF) at the level of spondylolisthesis and did not decompress cases of mild to moderate adjacent segment stenosis. We hypothesized that the demand for segmental hyperlordosis at the cranial adjacent segment to make lumbar spinal balance was decreased by posterior reduction and restoration of the SA at the spondylolisthesis level. The object of this study was to investigate the radiological changes at the cranial adjacent segment and compare clinical outcomes between patient with and without adjacent segment stenosis in patients with lumbar spondylolisthesis.
MATERIALS AND METHODS
1. Patients
After approval from the Institutional Review Board (Approval no. BLIND FOR REVIEW), consecutive patients who underwent single-level OLIF for L4-5 or L5-S1 lumbar spondylolisthesis (slip more than 3 mm) from December 2020 to February 2023 were retrospectively reviewed. A total of 40 patients (M:F = 12:28, age 66.6±10.4 years) were included in the analysis. Preoperative magnetic resonance imaging (MRI) scans were reviewed, and patients were divided into two groups based on mild to moderate central stenosis at the cranial adjacent segment (stenosis vs. no-stenosis groups). The stenosis grades were based on the separation degree of the cauda equina on T2-weighted axial images: grade 0 = no lumbar stenosis without obliteration of anterior cerebrospinal fluid space; grade 1 = mild stenosis with separation of all cauda equina; grade 2 = moderate stenosis with some cauda equina aggregated13). Lumbar central stenosis in the cranial adjacent segment was present in 16 patients (stenosis group) and absent in 24 patients. OLIF in one position was performed on all patients under the guidance of spinal navigation (OLIF-one). Postoperatively, patients were encouraged to ambulate from the day of surgery and discharged 3 to 4 days later. Indirect decompression was confirmed with MRI on postoperative day 1. Patients were scheduled to visit at 1, 3, 6, and 12 months postoperatively. This study had Institutional Review Board approval, and the need to obtain informed patient consent was waived.
2. Clinical and Radiological Parameters
Clinical parameters (numeric rating score of back pain [NRS-B, /10], leg pain [NRS-L, /10], and the Korean version of the Oswestry Disability Index [ODI, /100%]) and radiological parameters (pelvic incidence [PI], sacral slope [SS], pelvic tilt [PT], lumbar lordosis from L1-L5 [LL], C7-sagittal vertical axis [C7-SVA], SA at the index level [SA-index], SA at the adjacent segment [SA-cranial], horizontal distance of the index level from the S1-plumb line [distance], and the spinal canal area at the index level [Area-index], and adjacent level [Area-cranial]) were longitudinally compared between groups (Fig. 1). The radiological measurements were measured without information about patients and groups in 200% magnified images by a blind reviewer.

Radiological measurements. (A) Pelvic parameters (pelvic incidence [PI], sacral slope [SS], and pelvic tilt [PT]) were measured from the center of both femur heads to the center of the upper endplate of S1. Lumbar lordosis (LL) from L1-5, segmental angle (SA) at the index level (SA-index), and SA at the cranial adjacent segment (SA-cranial) were measured using Cobb’s method. The horizontal distance of the index level from the S1-plumb line (distance) and C7-sagittal vertical axis (C7-SVA) were measured from the center of the upper vertebral body of spondylolisthesis and center of C7 to the vertical line of the posterior superior corner of S1. (B) The area of the spinal canal was measured in an axial image.
3. The Surgical Procedure of OLIF-one
The patient was placed in a 90° right lateral decubitus position under general anesthesia. The patient was located at the lateral margin of the table to facilitate the insertion of pedicle screws in the lateral position (Fig. 2). Percutaneous pedicle screws (Longitude; Medtronic, Memphis, TN, USA) were inserted posteriorly under spinal navigation guidance (O-arm surgical navigation; Medtronic). After inserting the pedicle screws, the anterolateral lumbar disc was approached via an anterior retroperitoneal trajectory under the guidance of spinal navigation. The disc space was cleared with Cobb’s elevator, reamer, and curettes. After the preparation of cranial and caudal endplates, serial trial cages were inserted to restore disc height. The insertion of serial trial cages loosened the tight disc space and facet joint and made the spondylolisthesis mobile. Next, the spondylolisthesis was reduced with the pedicle/screw system. After spondylolisthesis reduction, set screws were not inserted to allow the vertebra to slide along the rod during insertion of the interbody cage. Anteriorly, the anterior margin of the cranial and caudal vertebra was identified under surgical vision, and the disc space was cleaned again. The interbody cage was then inserted into the disc space. Thereafter, the pedicle screw/rod system was finally assembled with set screws.
4. Statistical Analysis
All continuous data were presented as mean ± standard deviation, and non-continuous data were presented with numbers (proportion). Continuous parameters were compared with Student’s t-test or Mann-Whitney U test, and non-continuous parameters were compared with the χ2 test. Patients’ demographic characteristics (age, sex, body mass index [BMI; kg/m2], surgical level [L4-5 vs. L5-S1]), clinical parameters, and radiological parameters were compared between groups. Clinical and radiological parameters were longitudinally compared within and between the groups using a linear mixed-effect model. The fixed effects were the group, time (1, 3, 6, and 12 months after the operation), the interaction between group and time, preoperative parameters, and patient’s age, sex, BMI and the level of spondylolisthesis if those were statistically significant variables. The random effect was the subject. If the overall time effect was significant in the mixed-effect model, the difference between times was compared using the Bonferroni method. All analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA), and significance was defined as p less than 0.05 (two-tailed).
RESULTS
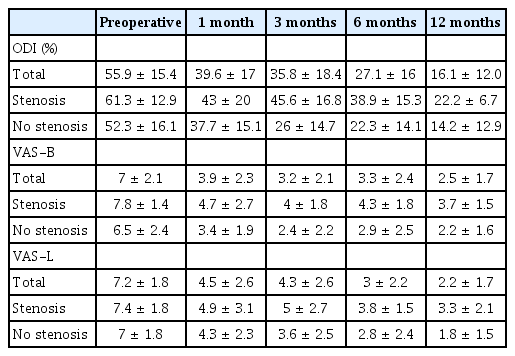
The demographics are described in Table 1. Although statistically insignificant, patients in the stenosis group were older than patients in the no-stenosis group (mean 70.3 vs. 64.2 years, p = 0.07). The preoperative clinical and radiological parameters were not significantly different between groups except for C7-SVA (p > 0.05; Table 1), which was significantly higher in the stenosis group than in the no-stenosis group (56.7 mm vs. 25.6 mm; p = 0.01; Table 1). Postoperatively, clinical outcomes (ODI, VAS-B, and VAS-L) significantly improved from postoperative 1 month (p < 0.01 in both stenosis and no-stenosis group), and the improvement was maintained during the follow-up period (mean 7 ± 5 months) without a significant difference between groups (p > 0.05; Table 2, Fig. 3). SA-index significantly improved in both groups (p < 0.01 in both groups), while SA-cranial improved only in the stenosis group (p < 0.01; Table 3). Area-index significantly improved from 156.0 ± 110.6 mm2 to 203.5 ± 107.6 mm2 in the stenosis group (p < 0.01) and from 117.1 ± 126.8 mm2 to 168.5 ± 122.0 mm2 (p < 0.01) in the no-stenosis group after surgery. An increase in Area-cranial was observed in the stenosis group (from 146.0 ± 55.8 mm2 to 164.9 ± 52.0 mm2; p = 0.003), but not in the no-stenosis group (from 175.6 ± 44.0 mm2 to 176.8 ± 43.0 mm2; p = 0.15). The distance from S1 plumb significantly decreased in both groups at postoperative 1 month (p < 0.01), and this decrease was maintained during the follow-up period without a significant difference between groups (p > 0.05). LL and PI-LL significantly improved in both groups (p < 0.01) at postoperative 1 month, and this improvement was maintained through the follow-up period (p > 0.05). C7-SVA improved in the stenosis group (p = 0.005), but not in the no-stenosis group (p = 0.11). Other parameters did not differ significantly between groups (p > 0.05). Complications occurred in 6 patients (postoperative ileus, 3; left leg transient dysesthesia, 1; transient left hip weakness, 1; pseudo-hernia around skin incision, 1) in the stenosis group (37.5%) and 7 patients (left leg transient dysesthesia, 4; transient left hip weakness, 2; vascular injury, 1) in the no-stenosis group (29%); there was no significant difference in the incidence of complications between groups (p = 0.59).

Outcomes. (A) Mean values of the Oswestry Disability Index (%). Standard deviations are marked with vertical lines. (B) Mean values of the numeric rating pain score of back pain (/10). (C) Mean values of the numeric rating pain score of leg pain (/10).
Case Illustration
A 74-year-old male patient visited with intermittent neurogenic claudication (distance 100 m) for 3 years (ODI/NRS-B/NRS-L, 71%/10/7). MRI and X-rays showed spondylolisthesis at L4-5 and moderate stenosis at L3-4 (Fig. 4). OLIF-one surgery was performed at L4-5, and postoperative MRI showed realigned spondylolisthesis at L4-5 and improved stenosis at L3-4. The preoperative SA at the index level (L4-5) was 16.2°, increasing to 18°. The distance from the S1 plumb line decreased from 41 to 35 mm. SA-cranial changed from 9° to 4°. In postoperative 1 month, the patient could walk more than 2 km (ODI/NRS-B/NRS-L, 40%/5/4).

Preoperative and postoperative images. (A) Preoperative magnetic resonance imaging (MRI) shows spondylolisthesis at L4-5 and moderate stenosis at L4-5. The ligamentum flavum at L4-5 is buckled (arrow). (B) Postoperative MRI shows re-aligned spondylolisthesis at L4-5 and disappearance of buckling at L3-4 (arrow). (C) Preoperative X-ray shows spondylolisthesis at L4-5. The preoperative segmental angle (SA) at the index level (L4-5) was 16.2° and the distance from the S1 plumb line was 41 mm. (D) Postoperative X-ray shows re-aligned spondylolisthesis at L4-5. The SA at the index level increased to 18° and the distance from the S1 plumb line decreased to 35 mm. The SA at the adjacent segment changed from 9° to 4°.
DISCUSSION
The objective of this study was to compare the influence of mild to moderate stenosis at the adjacent segment after surgery only for spondylolisthesis between patients with and without adjacent stenosis. The SA at the adjacent segment decreased, and Area-cranial increased only in the stenosis group. The clinical outcomes were not affected by the presence of preoperative adjacent segment stenosis. We hypothesized that the demand for segmental hyperlordosis at the cranial adjacent segment to make lumbar spinal balance was decreased by posterior reduction and restoration of the SA at the spondylolisthesis level (Fig. 5). Although the issue of preexisting adjacent segment stenosis is still ongoing, the current study showed a natural improvement of mild to moderate stenosis at the adjacent cranial segment after reduction of spondylolisthesis, and the hypothesis has not been presented. This information may be helpful in deciding surgical extent, especially for patients with spondylolisthesis1,2,4,9,11,19,21,25,27).
Hypothesis of decreased demand for segmental hyperlordosis at the cranial adjacent level. This diagram shows spondylolisthesis at L4-5 with decreased disc height, segmental angle (SA), and anterior slippage. Hyperextension is observed at L3-4 to make a balanced lumbar spine. The bold arrows represent the direction of spondylolisthesis reduction during surgery (left). After reduction of spondylolisthesis, the requirement for segmental hyperlordosis at L3-4 decreases, and the upper lumbar spine rotates anteriorly (curved arrow) to balance the lumbar spine (middle). Finally, lumbar spine is balanced, with a decreased SA at L3-4 (right).
1. Surgical Treatment of Lumbar Spondylolisthesis
When nonsurgical treatment failed, surgical treatment was recommended for patients with spondylolisthesis3,5). Surgical treatment includes decompression only or decompression and fusion.3,5) Usually, adding fusion was recommended when instability was also present or anterior slippage was more than 3 mm3,5). This study included patients with anterior slippage of more than 3 mm, and fusion surgery was indicated. The reduction of spondylolisthesis during surgery may be a matter of debate due to the difficulty of the surgical procedure and potential nerve root injury resulting from the reduction of spondylolisthesis33). When the spinal canal is directly decompressed in posterior lumbar interbody or transforaminal interbody fusion, reduction may not be essential. However, when the spinal canal and neural foramen are indirectly decompressed by restoring the disc and foraminal height (the main characteristics of OLIF), spondylolisthesis is reduced to the best extent by using a pedicle and rod system for effective indirect decompression6,10,14,22,24). Therefore, reduction was routine practice in the OLIF procedure. In the present study, decompression at the neural foramen and spinal canal was confirmed with postoperative MRI, and no case necessitated additional direct decompression.
2. Issues of Adjacent Segment Degeneration
ASD is a major cause for a second operation after lumbar spinal fusion surgery8,29). A systematic review revealed that the incidence of radiologically diagnosed adjacent segment degeneration ranged from 5.3% to 100% during 36 to 369 months of follow-up. The incidence of symptomatic ASD ranged from 5.2% to 18.5% during 44.8 to 164 months of follow-up21,32). Okuda et al.20) and Toivonen et al.29) demonstrated that the rates of radiologically assessed adjacent segment degeneration at 2, 5, and 10 years were 19%, 49%, and 79%, respectively, after primary posterior lumbar interbody fusion (PLIF) surgery. Several potential risk factors are linked to the progression of adjacent segment degeneration, such as age, genetic factors, pre-existing adjacent segment degeneration or stenosis, laminectomy at the adjacent level of fusion, osteoporosis, and poor sagittal balance8,29). In addition, remaining pre-existing adjacent segment stenosis may limit recovery after surgery for spondylolisthesis34). Because pre-existing adjacent segment degeneration may be a poor prognostic factor, the adjacent level may be decompressed or fused during surgery at the index level2,28).
However, pre-emptive decompression at the adjacent segment may not always help reduce ASD. Hikata et al.9) showed that simultaneous decompression surgery did not reduce the incidence of symptomatic adjacent segment degeneration. In addition, decompression surgery at the adjacent segment may cause iatrogenic instability and accelerate adjacent segment degeneration, ultimately leading to ASD1,16,23). Sears et al.27) and Lai et al.11) demonstrated that laminectomy at the adjacent level increased the relative risk of degeneration by 4 times and reoperation by 2.4 times compared with patients without laminectomy at the adjacent level. Regarding the influence of pre-existing mild stenosis at the adjacent segment, Matsumoto et al.17) also showed that the clinical recovery rate and reoperation rate were not significantly different between patients with and without simultaneous adjacent segment decompression.
3. Demand for Hyperextension Based on Spinal Alignment
Each lumbar segment contributes to lumbar lordosis12,26). Essentially, the demand is normally distributed across multiple functional spine units (FSUs)12). However, when a segment malfunctions, the demand is concentrated on the other FSUs, especially on the adjacent level, and this seems to accelerate the degenerative process at the adjacent level23). Patients with ASD showed significantly smaller LL and SS and significantly larger PT than patients without ASD28). This finding implies that ASD may be affected by spinal balance28). The cranial adjacent segment may hyper-extend to compensate for the loss of segmental lordosis and anterior slipping due to spondylolisthesis. Therefore, the demand in the adjacent segment may decrease when spondylolisthesis and a decreased SA are restored after surgery (Fig. 5). Although this hypothesis was not verified in a longitudinal prospective study and mechanical stress analysis, the current study showed that the decreased demand improved the SA and spinal stenosis by the release of ligamentum flavum buckling. The untouched adjacent segment with mild to moderate stenosis did not influence the clinical outcomes. This finding may support the importance of realigning spondylolisthesis to reduce stress at the adjacent segment.
4. Advantages of Minimally Invasive Surgery
Mimura et al.18) showed that open PLIF had a 3.97 times higher risk (odds ratio, 3.97; 95% confidence interval, 1.02-15.48; p = 0.04) of developing ASD than minimally invasive PLIF. Approach-related factors may influence the development of ASD, along with other factors7,15,18,21,24). The advantage of minimally invasive pedicle screw fixation, which is the surgical technique of OLIF, is less injury to the multifidus muscle and medial branch of the dorsal ramus, which innervates the multifidus muscle15,18). Therefore, the advantage of reducing spondylolisthesis may be potentiated by reducing injury to the adjacent segment muscle and facet joints with minimally invasive surgery such as OLIF.
5. Limitations
Although this study presents a hypothesis regarding the ability of spondylolisthesis realignment to reduce demand at the cranial adjacent segment, it has several limitations.
First, this study was retrospective one, and the limited number of patients and retrospective design involve a risk of selection bias. In addition, considering that ASD occurs several years after surgery, the short-term follow-up period was a critical limitation. Therefore, the current results and hypothesis warrant a long-term follow-up study. Second, although there were no statistically significant differences in clinical outcomes, the scores of clinical parameters in the stenosis group were higher than those in the no-stenosis group. Despite a similar extent of improvement, the high scores may reflect the influence of mild to moderate stenosis at the adjacent segment. A long-term follow-up prospective study is necessary to see whether the score gap would be narrowed with time. Third, this study included surgical levels of L4-5 and L5-S1, and the biomechanics at cranial adjacent segments may vary at different surgical levels. Fourth, the hypothesis of this study has not been presented or studied with finite element analysis. Despite those limitations, we suggest these findings warrant a further multi-center study. Considering patients’ specific conditions (mild to moderate stenosis in the adjacent segment and spondylolisthesis), patients need to be recruited from multiple centers to have a robust suggestion, and we are anticipating to organize a prospective study among doctors with a similar philosophy. The subsequent study would give a better idea of how to address mild to moderate stenosis at an adjacent segment in patients with spondylolisthesis.
CONCLUSION
When mild to moderate lumbar spinal stenosis is present at an adjacent segment in patients with spondylolisthesis, it may not be essential to include the adjacent segment in surgery. Realigned spondylolisthesis may reduce the demand for adjacent segments for segmental hyperlordosis, thereby exerting a protective effect on ASD. However, the hypothesis should be verified by a randomized controlled trial with a long-term follow-up period and a large number of patients from multiple centers.
Notes
No potential conflict of interest relevant to this article was reported.Conflict of Interest.
FUNDING
This study was supported by grant no. 04-2021-0540 and 30-2023-0120 from the Seoul National University Hospital research fund. This study was supported by the Doosan Yonkang foundation (800-20210527).
Acknowledgements
The authors appreciate the statistical advice provided by the Medical Research Collaborating Center at Seoul National University Hospital.