A New, Effective, Safe, and Accurate Method of Cervical Selective Nerve Root Block
Article information
Abstract
Objective
Cervical selective nerve root block (SNRB) is an effective procedure that has long been performed for patients with radiating pain or paresthesia. However, there are several delicate structures around the cervical nerve root, damage to which could lead to irreversible neurovascular injury. Therefore, cervical SNRB requires a high skill level and extensive experience to execute it safely. To overcome these disadvantages, we used biplane computed tomography (CT)-guided fluoroscopy and a needle guidance program to achieve symptom improvement in a safer and shorter procedure. This study aimed to investigate the new method and report on its excellent clinical effects.
Methods
A total of 57 patients who experienced radiating pain due to cervical spinal stenosis resulting from a herniated disc were enrolled. From September 2020 to September 2021 subjects underwent a biplane CT-guided fluoroscopic nerve block at an outpatient clinic. All procedures were performed by biplane CT-guided fluoroscopy. We analyzed treatment effects with a numerical rating scale (NRS) at 2 and 4 weeks after the procedure. Logistic regression was performed to reveal the significance of changes in NRS after the injection.
Results
Pain improved in 56 of 57 patients (98%) after 2 and 4 weeks of follow-up compared to pre-injection pain. At the 2-week follow-up, the mean reduction based on NRS scores was 3.226 (2.782-3.674, 0; 95% confidence interval [CI], p < 0.001) indicating a 48% decrease in pain scores compared with the initial NRS. The mean reduction in NRS 4 weeks after the procedure was 3.544 (3.090-3.998, 0; 95% CI, p < 0.001) indicating a 52% reduction compared with the initial NRS. The average duration of the procedure was 4 min.
Conclusion
We demonstrate a clinically effective, safe, and accurate method using a biplane CT-guided fluoroscopy and needle guide program. This new method can be an easy and relatively uncomplicated alternative to treatment for patients with cervical radiculopathy and provides safe and accurate targeting, making it easy for inexperienced surgeons.
INTRODUCTION
Cervical radiculopathy occurs in 0.08% of the healthy population annually1). In terms of causes of compression to the cervical nerve root, 70% to 75% occur from cervical spondylosis and 20% to 25% from disc herniation14). Cervical radiculopathy is caused by a complex pathophysiology in stenosis of the cervical nerve root foramen2). Nerve roots and vessels are vulnerable due to the lack of perineurium and underdeveloped epineurium17). Within the stenosis foramen, the pressure rises and the function of the venous plexus around the root nerve declines, resulting in ischemia, which causes edema and increases the pressure6,9). Due to the physical pressure of the foramen for an extended period, inflammation and fibrosis around the nerve root progresses, resulting in radiculopathy13).
Patients suffering from radiating arm pain and paresthesia of cervical origin have usually been treated with nerve blocks since William Stewart Halsted first performed cervical plexus blocks at Bellevue Hospital in New York in 188411). Due to procedural efficacy, the cervical selective nerve root block (SNRB) has gained popularity and is now performed all over the world. Over time different methods have been introduced to improve its accuracy and safety and studies have reported various methods of cervical SNRB. Cervical SNRB via fluoroscopy-guidance is one of the most common methods used to visualize real-time contrast injection. Computed tomography (CT)-guided cervical SNRB provides better anatomical insight and avoids undesirable outcomes. Cervical SNRB performed under ultrasound also ensures precise needle control and soft tissue visualization of vessel and nerve structures17). However complications still include spinal cord injury and cerebral or spinal cord infarction, which can result in death12). Due to the critical anatomic structures around the cervical area, every cervical SNRB procedure requires accuracy to avoid medical complications. The purpose of this study was to introduce a safe and effective cervical SNRB method by targeting the nerve root precisely using biplane CT-guided fluoroscopy and needle guidance.
MATERIALS AND METHODS
A retrospective analysis was carried out using the picture archives and communication system (PACS) and electronic medical records of our hospital. Patients who received a cervical SNRB from September 2020 to September 2021 were reviewed. All procedures were performed by a single skilled neurosurgeon using the iGuide-Needle guidance program of Siemens Artis zee biplane angiography (Siemens, Erlangen, Germany) system, VC14. The analysis included all patients with a pre-procedural report and 2 to 4 weeks of post-procedural follow-up. The efficacy of the procedure was evaluated using a numerical rating scale (NRS) initially and followed up at 2 and 4 weeks.
The procedures were performed after obtaining patients’ written informed consent and were mainly performed on patients with radiculopathy, while patients with motor weakness were excluded because they were indicated for surgery. All patients were evaluated via cervical magnetic resonance imaging within a month prior to cervical SNRB, to identify the primary defect in the neural foramen and establish the cervical anatomy including the vertebral artery and structures nearby.
Patients were held in supine position on the fluoroscopy table with their necks turned 45º to the opposite side of the target (Fig. 1). Using the biplane CT-guided fluoroscope, we initially reconstructed a 3-dimentional CT image of the cervical spine and its surrounding structures (Video 1). Thus, we created a safe needle pathway including the precise entry point, target point and determined the depth of the target using the machine’s needle guiding program (Video 2). The actual entry point and target point were instructed by the guide program during live fluoroscopy screening that showed us the exact trajectory of the needle (Fig. 2). Since the procedure is carried out in biplane fluoroscopy the needle tip can be observed during the procedure on anteroposterior (AP) view of the cervical area. This enables the physicians to safely determine the safe depth of the needle. Once the needle pathway was established, 1 mL of contrast dye (Visipaque, Iodixanol) was slowly injected to outline and confirm the nerve root. When the nerve root was localized, an injection consisting of 2 mL of normal saline, 0.5 mL of dexamethasone and 0.5 mL of 20% lidocaine was administered. Following the procedure, patients were observed for 30 min for any adverse reactions before discharge. All procedures were performed without sedation so we could immediately manage patients with possible complications or complaints.

Patient positioned on the fluoroscopy table with his neck turned 45º to the contralateral side of the target.
The actual needle entry point can be seen during the live fluoroscopy screen with a virtual line in green under needle guidance.
Data Analysis
The collected data were analyzed with IBM SPSS statistics version 29 (SPSS Inc., Chicago, IL, USA) for Windows. Paired t-test was used to identify statistically significant differences in NRS between before and after cervical SNRB procedures during the follow-up period. The results were considered significant if the p-value was less than 0.05.
RESULTS
A total of 57 patients including 35 males and 22 females, were treated with the new cervical SNRB method from 2020 to 2021. The patients’ age ranged from 18 to 77 years. The mean initial and follow-up NRS scores were 6.75 (range, 5-9) and 3.53 (range, 1-7), respectively.
Forty-two patients received a single-site injection, and 15 patients underwent SNRB at multiple sites. The most common injection site was the C6 nerve root (37%), followed by C7 nerve root (32%) (Table 1).
Pain improved in 56 patients (98%) after weeks 2 and 4 of follow-up. One patient reported no change. The mean reduction in NRS scores at the 2-week follow-up was 3.226 (2.782-3.674, 0; 95% confidence interval [CI], p < 0.001) indicating a 48% reduction in pain score compared to prior. The mean reduction in NRS at 4 weeks after procedure was 3.544 (3.090-3.998, 0; 95% CI, p < 0.001) indicating a 52% decrease compared with the initial NRS (Table 2).
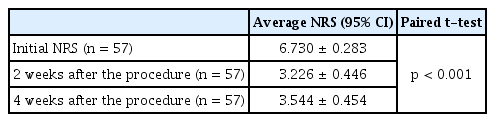
Difference of numeric rating scale between initial and after cervical selective nerve root block procedures
Two of the 57 patients (4%) expressed mild and transient complications, including palpitations and dizziness, which were successfully treated with supportive care in 30 min. The average procedural time was four min, with a minimum of three minutes and a maximum of seven min (Table 3).
DISCUSSION
Scanlon et al.14) reported 78 cases of complications including fatal outcomes among 287 ultrasound physician members of the American Pain Society, from 1990 to 2007. Physicians may be reluctant to perform what can be very effective injections due to the risk of severe complications associated with the anatomy of the structures near the neural foramen. Many methods have been proposed to support accurate and safe injection.
1. Fluoroscopy-guided Block via a C-arm
In this method, patients are held in a supine position and the C-arm is placed at a 45º oblique angle to identify the targeted cervical foramen. The operator can access the target nerve root from the lateral side of the cervical spine, usually the posterior border of the sternocleidomastoid muscle to the posteromedial aspect of the superior articular process. The needle is gently pushed 1 to 2 mm ventromedially into the posterolateral portion of the foramen. Before contrast injection, the AP view should be reviewed to determine the needle depth. After confirming the nerve root, a steroid injection is administered5) and the approximate procedure time is 15 min15).
Although fluoroscopy-guided cervical SNRB is a widely used procedure, blind insertion of the needle can increase the possible risk of injury to vital organs surrounding the neural foramen18). The risk of excessive needle insertion can lead to life-threatening consequences and the complication rate is very high at 19.4%4). The most serious complications result from intravascular injection-related irreversible nerve injury1).
2. Ultrasound-guided Nerve Block
Cervical SNRB under ultrasound guidance is performed in patients in a lateral decubitus position. Physicians determine the level of the cervical spine under ultrasound by comparing the shape of the vertebral body. A linear-high frequency ultrasound probe is placed transversely on the main side of the neck to obtain an axial view of the target, followed by scanning of the neural foramen of the targeted nerve root. By shifting the probe cranially, the space between the nerve root and the posterior part of the foramen can be visualized and used as a needle target. In the traditional approach, the needle tip is advanced to the target foramen in the anterolateral to the posterior direction, followed by fine aspiration20). Depending on the skill of the operator, it takes about 10 min16).
The biggest benefit of ultrasound-guided cervical SNRB is that injection can occur while viewing real-time images without radiation, while minimizing blood vessel damage via use of color Doppler mode7). In addition, it has the advantage of avoiding the side effects of contrast media. It can also be performed in a narrower space than with C-arm fluoroscopy5). However, this procedure requires expertise in ultrasound, which has a long learning curve. Further, any congenital anomaly involving the cervical area can interfere with the procedure. In obese patients with a very short neck, the accuracy of the procedure is reduced due to the deterioration of image quality16). Since the 3rd and 4th cervical transverse processes, which serve as markers, are very small, it is difficult to distinguish them, and the 8th cervical root is difficult to approach due to the clavicle5,7).
3. CT-guided SNRB
CT-guided cervical nerve block differs substantially from previous methods. The patient is held in the prone position with the head in a straight line, and the forehead is supported on a pillow. Using a CT scout view, the cervical level is marked, and the desired cervical neural foramen is delineated. The entry point is chosen to avoid important vessels such as carotid and jugular arteries and facilitate the approach to the outer foramen. Partial insertion of a straight spinal needle and minimal exposure of the CT scanner can be used to reveal the depth of introduction. After acquiring the initial image, the operator adjusts the needle to advance toward the posterior aspect of the neural foramen via intermittent CT imaging. Similar to the other procedures, the contrast is injected to confirm the target, followed by steroid injection7).
CT images provide high-resolution localization of anatomical structures such as blood vessels, soft tissue, and bony structures19). This information before the procedure allows for successful execution by accessing the needle in the correct pathway and positioning the needle tip delicately. However, since it is not a procedure that can be controlled in real-time, there are still risks, and there have been attempts to use a dorsal approach to avoid intravascular injection19).
4. Monoplane Fluoroscopy Guided SNRB
Using monoplane fluoroscopy for SNRB can effectively reduce patient symptoms. The patient is held supine on the fluoroscopic table with the chin rotated 30º away from the injection site. To prevent the patient from moving during the procedure, their head is held firmly with adhesive tape. Initial fluoroscopy is used to determine the precise fluoroscopic axis for the needle approach and to mark the needle placement site. The needle is then advanced in the caudal-to-cephalad direction to the lower lateral aspect of neural foramen after contrast is administered15). The procedure time of monoplane fluoroscopy-guided cervical SNRB has been reported to take about 6 min8).
This method is similar but more efficient than the SNRB via C-arm. Compared to cervical SNRB using only fluoroscopy, multi-slice CT enables more accurate root selection3). This is because high-quality preoperative images are easy to understand for each patient's anatomy10). In addition, real-time injection is possible so that intravascular injection can be prevented. In one study, these advantages completely prevented major complications, and minor complications only occurred 5.5% of the time10).
5. Cervical SNRB via Biplane CT-guided Fluoroscopy and Needle Guidance
We introduce a new technique for SNRB via biplane CT-guided fluoroscopy and needle guidance. Compared with previous methods, our new technique has numerous advantages. The advantages of previous methods were that high-quality pre-procedure images could be obtained with 3-dimensional (3D) CT and fluoroscopy confirmed in real-time, intra-procedure. A minimum 3D CT plane is used to reconstruct important structures around the target area and minimize vessel injury. The short 3D CT reconstruction time minimizes artifacts of breathing or movement. The use of biplane fluoroscopy provides AP and oblique views simultaneously, resulting in a high degree of safety.
By using the guided needle, we can establish a safe needle pathway to ensure accurate selection of the target neural foramen. Its high accuracy saved the need for several needle repositioning often seen in previous methods. The entire procedure is very easy to learn because the needle guidance shows the direction of injection in an intuitive way. In fact, in our class we found that even residents with little experience with nerve block were able to easily perform the procedure.
Objective comparison is difficult because the procedure time depends on the patient's cooperation and anatomical difficulty. But we believe the procedure time is less or similar compared to other methods even with the 3D reconstruction process.
6. Limitation
There are several limitations to this study. The retrospective study design has inherent limitations. Also, a relatively small number of cases and short follow-up periods limit the generalizability of the findings and can lead to false-negative results. Additionally, we could not compare patients’ symptoms with other procedures to establish the efficacy of our technique. The amount of radiation exposure, which can be considered as a disadvantage of this procedure, has not been investigated and in future studies this aspect must be taken into consideration. Also, because this method needs both 3D CT reconstruction and a biplane fluoroscopy machine, the cost can be another disadvantage in other countries, however, in our institute there were no differences.
CONCLUSION
Combining biplane CT-guided fluoroscopy with cervical SNRB under needle guidance is more precise than previous methods. It minimizes patients’ symptoms and ensures their safety. Using a guided needle, the technical utility and safety can be easily adapted to different patients to enhance procedural outcomes. The findings demonstrate the safety and effectiveness of the new method.
Notes
No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIAL
Supplementary materials are available at https://doi.org/10.21129/nerve.2023.00423
Supplementary Video 1.
Initial 3-dimensional computed tomography scan for the cervical spine and surrounding structures.
Supplementary Video 2.
Needle guidance for precise and safe entry, as well as target depth.

