Outcome of Decompressive Laminectomy with or without Posterior Screw Fixation for Thoracic Ossification of the Ligamentum Flavum with Disc Degeneration
Article information
Abstract
Objective
Thoracic myelopathy caused by the ossification of the ligamentum flavum (OLF) is commonly treated with surgical decompression. This study aimed to compare the clinical and radiological outcomes of surgical decompression without posterior screw fixation (decompressive laminectomy [DL] group) and with posterior screw fixation (laminectomy with screw fixation [LSF] group) for thoracic myelopathy due to OLF with disc degeneration.
Methods
A retrospective review of 35 patients (DL group, n = 19; LSF group, n = 16) was conducted. Clinical variables (Japanese Orthopaedic Association scores) and radiological variables (including sagittal vertical axis, pelvic tilt, thoracic kyphosis, sacral slope, lumbar lordosis (LL), segmental Cobb’s angle, dynamic Cobb’s angle, and dynamic thoracolumbar junction [dTLJ] at the operated level) were measured preoperatively and 1 year postoperatively.
Results
Both groups exhibited significant improvements in clinical characteristics postoperatively. LL significantly increased at 1 year postoperatively in both groups. Other sagittal alignment parameters did not change significantly. The dTLJ did not differ significantly between the groups preoperatively; however, the dTLJ of the DL group was larger than that of the LSF group at 1 year postoperatively. There was no significant difference between the groups’ dynamic Cobb’s angles or risk of complications.
Conclusion
Decompression surgery for OLF resulted in clinical improvement regardless of whether posterior fixation was performed. Decompression without posterior fixation could allow thoracolumbar motion preservation and might be an effective approach for thoracic OLF with disc degeneration.
INTRODUCTION
Ossification of the ligamentum flavum (OLF) leads to thoracic spinal cord compression from fibrosis and calcification9). The prevalence of OLF is higher in Asian populations, and it is often an indication of surgical decompression due to spinal cord disorders. The exact cause of OLF is not fully understood, but it is believed to be influenced by a sedentary lifestyle, cumulative micro-movements of the ligamentum flavum, and certain genetic factors9).
The therapeutic efficacy of decompression surgery for OLF has been recognized in several studies8). However, there is insufficient evidence regarding which patients specifically require additional screw fixation. Previous studies have shown that screw fixation is often chosen for patients with severe symptoms8). When there is relative instability, screw fixation may be considered; however, there is uncertainty regarding the choice of fixation when there are degenerative disc changes.
We aimed to analyze the clinical and radiological outcomes of patients with degenerative disc changes who underwent either standalone decompression surgery (decompressive laminectomy [DL]) or decompression surgery with screw fixation (laminectomy with screw fixation [LSF]).
MATERIALS AND METHODS
1. Patient Selection
Patients with myelopathy due to thoracic OLF—with disc degeneration rated as Pfirrmann’s grade 4 or 5 and who had undergone posterior decompression surgery between January 2012 and September 2022—were retrospectively enrolled from an institutional clinical data warehouse16). Eligible patients were those with a minimum follow-up duration of at least 12 months. The exclusion criteria were a history of cervical spondylosis, a tumor or infection, or previous deformity correction surgery. This study was approved by the Institutional Review Board of Chonnam National University Hospital (Approval no. 2023-292).
2. Surgical Technique
Surgical procedures were performed by two spine surgeons who had experience with more than 500 spine surgeries. Before 2018, OLF and the residual ligamentum flavum were removed after laminectomy with facet preservation (DL group). From 2018, posterior transpedicular screw fixation on the segment of the OLF was routinely performed after OLF removal (LSF group). All patients were encouraged to ambulate from the day after surgery and were discharged 9 to 11 days postoperatively. Patients in the LSF group were requested to wear a thoracolumbar orthosis for a month.
3. Clinical Assessment
The clinical assessment included patient-reported outcome measures collected from the electronic medical records and clinical data warehouse. The modified Japanese Orthopaedic Association (mJOA) score for neurological function was evaluated preoperatively and 1 year postoperatively10).
4. Radiologic Assessment
Thoracic lateral radiographs in the flexion and extension postures were obtained preoperatively and 1 year postoperatively. To evaluate dynamic movement, the difference between Cobb’s angles in the flexion and extension postures of the surgical segment was defined as the dynamic Cobb’s angle (dCA) (Fig. 1). The difference between Cobb’s angles in the flexion and extension postures of T10-L2 was defined as the dynamic thoracolumbar junction (dTLJ) (Fig. 1).

Radiological measurements of sagittal alignment and range of motion. (A) From whole-spine standing lateral radiographs, the following sagittal parameters were measured; (a) pelvic incidence, (b) lumbar lordosis, (c) sacral slope, (d) pelvic tilt, (e) thoracic kyphosis, (f) thoracolumbar slope, and (g) sagittal vertical axis. (B) To evaluate dynamic movement, the difference between the Cobb’s angles (CA) associated with the flexion and extension postures of the surgical segment was defined as the dynamic CA. The difference between CA in the flexion and extension postures of T10-L2 was defined as the dynamic thoracolumbar junction (TLJ).

Measurement of the canal compromise ratio from preoperative spine magnetic resonance imaging (MRI). (A) From the axial MRI at the upper disc level of the ossification of the ligamentum flavum (OLF) lesion, the cross-section area was measured along the border of the canal, and the area was taken as the canal area (white line). (B) From the axial MRI of the level most severely compressed by the OLF lesion, the cross-sectional area was measured along the border of the cord, and the area was taken as the cord area (dotted line). The percentage obtained by (canal area-cord area)/(canal area) × 100 was taken as the canal compromising ratio. The M6 software application (INFINITT, Seoul, Korea) was used for these calculations.
Whole-spine standing lateral radiographs were obtained preoperatively and 1 year postoperatively. As shown in Fig. 1, the following sagittal parameters were measured: sagittal vertical axis (SVA), pelvic incidence (PI), lumbar lordosis (LL), pelvic tilt (PT), thoracic kyphosis (TK), sacral slope (SS), and thoracolumbar slope (TLS).
Canal compromising ratios (CCRs) were measured using preoperative spine magnetic resonance imaging (MRI) (Fig. 2)2). From the axial MRI at the level above the OLF lesion, the cross-sectional area was measured along the border of the canal, and the area was taken as the canal area. From the axial MRI of the level most severely compressed by the OLF lesion, the cross-sectional area was measured along the border of the cord, and the area was taken as the cord area. The percentage of (canal area-cord area)/(canal area) was taken as the CCR. These measurements were taken using the M6 software application (INFINITT, Inc., Seoul, Korea).
5. Statistical Analyses
Comparisons of continuous variables were analyzed using the Mann-Whitney U test, whereas comparisons of non-continuous variables were analyzed using the χ2 test or Fisher’s exact test. A repeated-measures general linear model was used to compare the parameters of the DL group with those of the LSF group at admission and 1 postoperative year. All statistical analyses were performed using SPSS Statistics for Windows, version 27.0 (IBM Corp., Armonk, NY, USA), and statistical significance was defined as p less than 0.05.
RESULTS
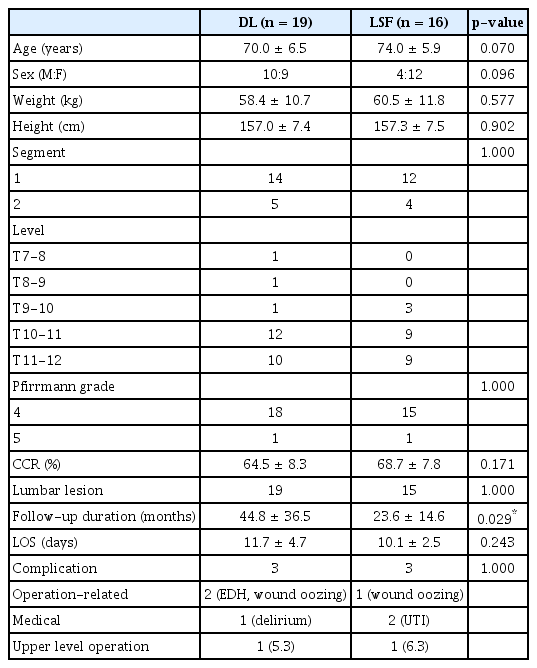
The characteristics of the patients are shown in Table 1. The DL group had an average age of 70.0 ± 6.5 years, whereas the LSF group had an average age of 74.0 ± 5.9 years. The DL group consisted of 10 men and 9 women, whereas the LSF group consisted of 4 men and 12 women. Statistical analysis did not show any significant differences in age or sex between the two groups. There was also no significant intergroup difference in Pfirrmann’s grade distributions. The CCR of the DL group was 64.5%, and that of the LSF group was 68.7%, but there was no statistically significant difference in this regard.
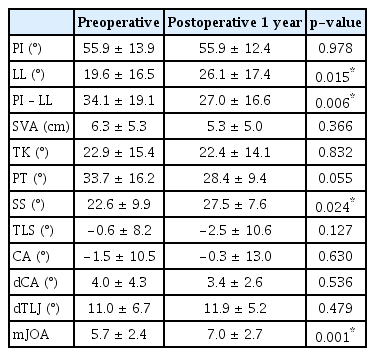
LL and SS increased significantly between the preoperative and 1-year postoperative evaluations (Table 2). Differences between the preoperative and 1-year postoperative PI, SVA, TK, PT, and TLS were not statistically significant. There were no statistically significant intergroup differences in the preoperative sagittal alignment parameters (Table 3). At 1 postoperative year, there were no significant intergroup differences in the sagittal alignment. In the subgroup analysis, both groups showed statistically significant improvement in LL and PI-LL, but there were no significant changes in the other parameters. The mean dTLJ movement was 14.0 ± 5.9° in the DL group and 9.9 ± 4.3° in the LSF group (p = 0.035). Moreover, there was no significant change in dCA (Table 3).
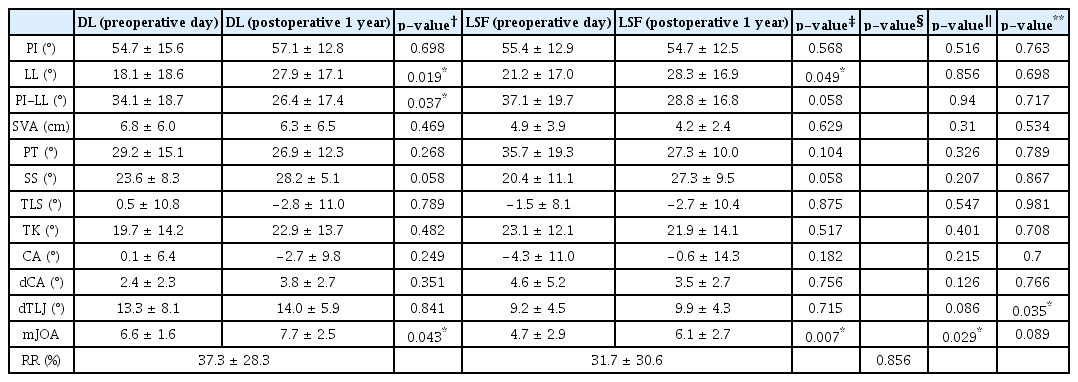
Comparison of preoperative and postoperative radiologic parameters and clinical outcomes between the DL and LSF groups
The mean preoperative and 1-year postoperative mJOA scores were 5.7 ± 2.4 and 7.0 ± 2.7, respectively, with a statistically significant improvement (Table 2). The mean preoperative mJOA scores of the DL and LSF groups were 6.6 ± 1.6 and 4.7 ± 2.9, respectively, with a statistically significant difference (p = 0.029) (Table 3). At the 1-year follow-up, the mean mJOA scores had improved to 7.7 ± 2.5 for the DL group and 6.1 ± 2.7 for the LSF group; however, the difference was not statistically significant between the two groups (Table 3). The mean mJOA recovery rates were 37.3% and 31.7% in the DL and LSF groups, respectively; these were not statistically significant.
In each of the two groups, there were three major complications that resulted in prolonged hospital stay. In the DL group, there was a revision procedure for a patient with an intraoperative epidural hematoma. During the follow-up period, each group had a single instance of OLF accompanied by upper-level myelopathy. These instances occurred at 4 years and 3 years postoperatively, respectively, and necessitated additional decompression surgery.
DISCUSSION
OLF was first identified in 1920 and is known to cause pain or myelopathy due to bony transformations within the yellow ligament. While the exact mechanisms responsible for this ossification remain poorly understood, a combination of mechanical stimuli as well as metabolic and biological factors are believed to contribute to cellular proliferation and matrix expansion9,11,17). Genetic factors have also been reported to influence OLF development4,17). The prevalence of thoracic OLF is up to 16.9%; however, not all patients need to undergo surgery14). Surgical decompression is required when myelopathy progresses, and the effectiveness of decompression surgery for OLF has been demonstrated in previous studies8). Various studies have reported sufficient treatment effects with only decompression surgery, and recurrence is uncommon6,8,15).
In some cases, a combined fixation technique has been used; however, given the pathophysiology potentially triggered by micro-movements or macro-movements, especially associated with partial facet removal during decompression, it may be reasonable to stabilize the motion via screw fixation after decompression1,5,6,13,18,20). Hwang et al.6) reported that screw fixation is beneficial for the progression of kyphosis in OLF. However, the need for fixation for specific patients is still controversial.1) In particular, OLF with ventral lesions has been reported only in the presence of ossification of the posterior longitudinal ligament12). In this study, we analyzed posterior decompression in OLF patients with degenerative thoracic disc changes.
Even when ventral compression was accompanied by disc degeneration of a grade higher than 4 on the Pfirrmann scale, the mJOA score was improved only by the removal of OLF. Throughout the follow-up period, there was no recurrence of symptoms in the treated segment for either group. Symptom improvement and progression prevention were achieved in both groups by removing the compressive lesion associated with myelopathic symptoms. Several studies have shown that recurrence is very rare, which is consistent with the results of our study1,7).
Most patients (97.1%) had degenerative changes in the lumbar spine with loss of LL and significant PI-LL mismatch preoperatively. Chang et al.3) found that thoracic OLF patients had hypolordotic spines with larger PI-LL mismatch than age- and sex-matched control patients with lumbar spondylosis. The radiographic results of our study showed that both groups had increased LL postoperatively. Although SS showed a mild improvement, the p-value did not reach statistical significance in the subgroup analysis. This lack of significance seems to have been due to the insufficient sample size in the subgroup analysis. After OLF removal—regardless of screw fixation—improvements in LL and mJOA scores were observed. The improvements in some sagittal alignment parameters, such as LL and SS, are presumed to have resulted from the patients’ improved ability to maintain a more upright posture due to pain reduction and partial recovery of lower extremity strength. Symptomatic improvement and postural correction may be attributed to the decompression itself rather than the effect of immobilization.
There was no significant difference in segmental motion between the two groups. Segmental motion of the lower thoracic area is known to be 9° to 10° per segment; however, it was around 3.7° per segment in our study. There was no difference in postoperative segmental motion with or without screw fixation. The mean dTLJs—reflecting the total motion angle of the thoracolumbar junction—were 13° and 9° in the DL and LSF groups, respectively, and the motion angle was more preserved in the DL group. Even in patients with disc degeneration, the rib cage and orientation of the facet joints appeared to maintain this stability. In the LSF group, the mobility of both the surgical segment and thoracolumbar junction was reduced preoperatively, and the same was observed after surgery. Although thoracic OLF has been associated with rotational motion, there have been no reports on the relationship between thoracic sagittal motion and OLF, and further studies are warranted13,19). Moreover, screw loosening was observed in two patients, which did not result in symptoms. The affected patients did not have any aggravated neurological symptoms during follow-up. In these cases, DL may be sufficient.
The possibility of progression of OLF at levels other than the surgically treated segment should be considered. After 3 and 4 postoperative years, additional operations were performed for proximal OLF in each group. In the screw fixation group, the mobility of both the surgical segment and thoracolumbar junction was decreased, and excessive stress was applied to the adjacent facet; thus, deterioration of the adjacent OLF should be considered.
This study had several limitations. First, it should be noted that the assignment of the participants to the two groups was not randomized, potentially introducing a selection bias. Moreover, the statistical power of the study might have been compromised by the relatively small sample size. Second, it was observed that there was no significant difference in sagittal imbalance between the treatment modalities; a comprehensive long-term follow-up study is warranted to validate this finding.
CONCLUSION
In comparison with LSF for thoracic OLF with disc degeneration, DL alone demonstrated comparable segmental motion preservation and clinical outcomes at 1 postoperative year. Decompression without posterior fixation could allow thoracolumbar motion preservation and might be an effective approach for thoracic OLF with disc degeneration.
Notes
No potential conflict of interest relevant to this article was reported.