Surgical Experience of Brachial Plexus Injury
Article information
Abstract
Objective
Brachial plexus injuries (BPIs) are complex and challenging injuries that can result in significant loss of functions involved in the upper extremity. The purpose of this study is to provide useful guidance for the management of BPIs.
Methods
Twenty-two patients who underwent intercostal nerve transfer (ICNT) only or ICNT with additional spinal accessory nerve transfer (SANT) by sural nerve graft interposition for traumatic BPIs from 2005 to 2014 were retrospectively studied. The Medical Research Council scale was used for outcome assessment. Follow-up was performed for at least 1 year to confirm neurological outcomes.
Results
Seventy-seven percent of all patients gained motor grade improvements after surgery; however, patients of the combined surgery group, who underwent ICNT and SANT (mean=2.2), showed better motor grade scale improvements than patients of the single-operation group, who underwent only ICNT (mean=1.083) (p=0.030). Moreover, a mean time to surgery of less than 6 months resulted in better outcomes than a mean time to surgery of greater than 6 months. Reinnervation of the musculocutaneous nerve was demonstrated in 92.8% of the patients who underwent surgery within the first 6 months postinjury, in 40% of the patients with a delay of between 6 and 12 months, and none of the patients who underwent surgery after 12 months (p=0.004).
Conclusion
This study validated that ICNT with SANT is more effective for reconstructing musculocutaneous nerves in patients with BPIs, along with the fact that surgery should be performed as soon as possible after injury at least 6 months.
INTRODUCTION
Brachial plexus injuries (BPIs) are often devastating and may include avulsion, stretching, or rupture of cervical nerve roots, resulting in significant disability8). Critical motor function in the limb may be lost, sensation in the hands may be impaired, and disabling pain may ensue. BPIs can affect individuals of any age and of either sex. Traumatic lesions usually arise from motor vehicle accidents and falls, and stretch injuries may also follow lesser damage such as stab injuries. Moreover, tumor irradiation is another cause of BPIs. Overall, the incidence of BPIs has rapidly increased due to technological advancements in transportation, resulting in a greater number of motor vehicle accidents.
Microsurgical treatment of BPIs has significantly advanced and can be used for the reinnervation of target muscles, resulting in new modalities to improve the clinical outcome of brachial plexus lesions. Treatment strategies are focused toward restoring shoulder stabilization, shoulder abduction, and elbow flexion. Many systematic reviews have been published in support of a preferred surgical treatment; however, the surgical management of BPIs remains a challenge. Four surgical procedures have been reported to improve functional outcome and are commonly used to repair BPIs: neurolysis, nerve repair, nerve grafting, and nerve transfer. Traditionally, brachial plexus surgery begins with nerve exploration to determine the pathoanatomy of the lesion, plan the strategy of nerve reconstruction, determine whether there is rupture or avulsion of each nerve root, and identify available donors and recipients. Despite improvements in surgical techniques, surgical outcome and functional restoration of the affected arm is still very limited10).
The strategies commonly used to reconstruct the brachial plexus mainly include peripheral nerve grafting and/or neurotization12). Neurotization of the brachial plexus is usually accomplished using the intercostal, accessory or in some cases, the phrenic nerve to reinnervate the musculocutaneous nerve for elbow flexion or the suprascapular nerve for shoulder abduction1,4,12).
In this study, we compared recovery of elbow function by reinnervating the musculocutaneous nerve after intercostal nerve transfer (ICNT) with or without spinal accessory nerve transfer (SANT) by sural nerve graft interposition in patients with traumatic BPIs. Functional outcome was analyzed to provide useful guidance for the management of BPIs.
MATERIALS AND METHODS
1. Patient Selection
We retrospectively selected 26 patients with severe BPIs who were surgically treated at the Department of Neurosurgery of the Soonchunhyang University Medical Center by reviewing medical records from 2005 to 2014. Among these patients, we selected those who met the following criteria: (1) presence of traumatic rupture or avulsion of the brachial plexus, (2) limited elbow flexion function, (3) failure of electrophysiological assessment to demonstrate signs of biceps reinnervation, (4) all surgeries performed by the same experienced surgeon, and (5) a postoperative follow-up period of at least 1 year. Based on these inclusion criteria, 22 patients (20 men, 2 women) were enrolled in this study. The majority of patients had sustained their injuries in traffic accidents. The age of the patients at the time of surgery ranged from 16 to 59 years (mean, 37.3 years), and the mean interval between injury and surgery was 17 weeks.
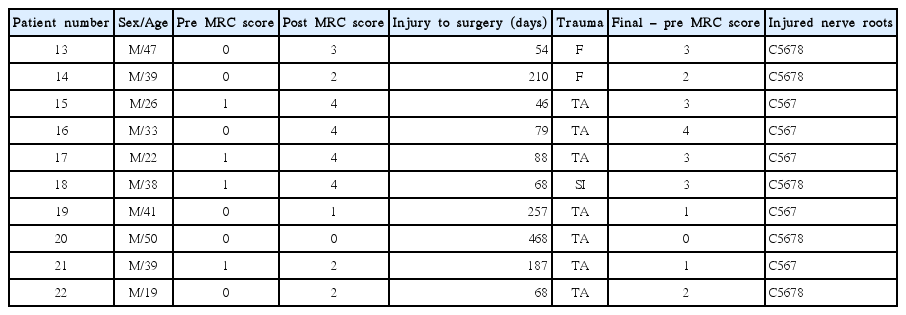
Patients were divided into two groups: the ICNT group (n=12) comprised patients who had undergone only ICNT (Table 1), and the SANT group (n=10) comprised patients who had undergone ICNT with additional SANT by sural nerve graft interposition (Table 2). Surgery was determined randomly in all patients.
To determine the influence of the time interval between injury and surgery, the patients were divided into three main groups: (1) a time interval of 1 to 6 months, (2) a time interval of 7 to 12 months, and (3) a time interval longer than 12 months.
2. Evaluation
Before surgery, all patients underwent needle electromyography examination. Computed tomography or magnetic resonance imaging was performed prior to surgery to detect root avulsions. Electrophysiological studies performed before and during surgery revealed injured nerve roots.
3. Preoperative and Postoperative Assessment
Prior to surgery, all patients underwent the manual muscle test (MMT) led by an independent observer who was not involved in the surgical procedure. Elbow flexion function evaluation was adapted from the Medical Research Council (MRC) scale for measuring muscle strength and was performed the day prior to surgery.
After surgery, each patient underwent the MMT at least once monthly for 1 year and yearly thereafter; results were evaluated using MRC scores. The final MMT scores for elbow flexion were also recorded using the MRC scale.
4. Surgical Techniques
Surgery was performed as follows in all patients. The patient was placed in the supine position with the affected arm placed at approximately 90 degrees of abduction onto an arm board. Intraoperative nerve monitoring was used for nerve identification and nerve injury assessment. Surgery was performed via a standard infraclavicular approach for nerve roots and the brachial plexus. A 7-cm incision was made from the distal two-thirds of the clavicle to the anterior deltoid grove. The lateral margin of the brachial plexus was located at least 25 mm distally from the clavicle midpoint, and the musculocutaneous and median nerves were exposed approximately 20 mm distal to the lateral margin of the pectoralis minor muscle5) (Fig. 1).
The musculocutaneous and median nerves were exposed at a point approximately 20 mm distal to the lateral margin of the pectoralis minor.
For ICNT, an arch-shaped incision was made across the chest from the midaxillary line to the sternal border, just inferior to the nipple. The intercostal nerves of the third to fifth ribs were identified, harvested along their course, and passed subcutaneously below the pectoralis minor muscle from the chest incision to the medial arm incision, where the musculocutaneous nerve was exposed. The three intercostal nerves were coapted to the musculocutaneous nerve using a suture (Fig. 2).

Intercostal nerve transfer (A) Harvesting the intercostal nerves. (B) Coapting with the musculocutaneous nerve.
For SANT, a 15-cm vertical incision was made 5 cm below the popliteal fossa to the midline of the gastrocnemius muscle. The sural nerve was identified beside the small saphenous vein and was dissected as required. The proximal sural nerve was sutured to the spinal accessory nerve, and the distal sural nerve was sutured to the distal musculocutaneous nerve (Fig. 3). Less than 5 cm of the sural nerve was used. SANT was performed three days after ICNT.
5. Statistical Analysis
Outcomes in weeks were expressed as the mean and standard deviation and compared using a nonparametric test. Age at surgery, numbers of injured nerve roots, preoperative and final MRC scores, and changes in MRC scores were compared between the ICNT and SANT groups using the Mann-Whitney nonparametric U test. The three groups representing the different time intervals between injury and surgery were compared using the Kruskal-Wallis test. The relationship between the time interval from injury to surgery and the surgical result was evaluated using linear regression analysis. Statistical significance was indicated by p<0.05.
RESULTS
1. Postoperative Results
The mean age of the patients at the time of surgery, mean time interval between the injury and surgery, number of injured roots, and preoperative MMT were not significantly different between the ICNT and SANT groups. Moreover, the causes of trauma were similar between the two groups.
The mean final MRC scores for elbow flexion in the ICNT and SANT groups were 1.42 and 2.60 (p=0.05), respectively. The average nerve transfer and combined group-obtained MRC scores after surgery were 1.083 and 2.20 (p=0.03), respectively. The group that underwent both ICNT and SANT had-significantly better outcomes than the group that underwent only ICNT. In terms of functional recovery, 77% of patients had improved MRC scores, 32% achieved an MRC score of at least 3, and 18% attained a score of at least 4(Table 3). Box- and-Whisker plot of relationship between change of MRC and ICNT/SANT group is shown (Fig. 4).
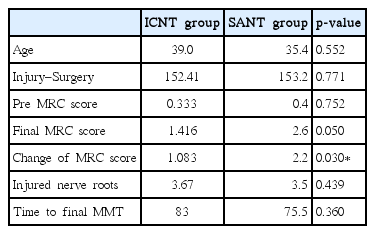
Average values and statistics of the intercostal nerve transfer and spinal accessory nerve transfer groups
2. Preoperative Time Interval
Postoperative outcomes according to the time between injury and surgery were better for patients who underwent surgery soon after the injury, regardless of the surgical procedure performed. Comparisons between the different time intervals demonstrated that patients with a preoperative time interval of 1 to 6 months achieved a significantly better recovery rate (92.8%) than patients who underwent surgery from 7 to 12 months (40.0%) or after 12 months (0.0%) (p=0.004) (Table 4). Indeed, our results demonstrated significantly impaired functional outcomes in patients who underwent surgery more than 12 months after injury (Fig. 5).
Scatterplot of linear regression analysis showing the relationship between the time interval from injury to surgery and the surgical result (Medical Research Council scale score). For the most part, the best outcomes were obtained in patients who underwent surgery within 6 months of injury. MRC, Medical Research Council (R square: 0.574, Constant: 3.180).
DISCUSSION
Most BPIs result from closed traction injuries that affect the supraclavicular plexus and the C5, C6, and C7 nerve roots, resulting in lack of shoulder and elbow functions. C5 and C6 root involvement results in significant problems with shoulder abduction, external rotation, elbow flexion, and forearm supination, while C7 root involvement may lead to additional deficits involving finger, wrist, and elbow extension.
There are two types of characteristic lesions seen in BPIs: avulsion and rupture. Avulsion refers to a nerve torn from its attachment, while rupture refers to a nerve injury involving a traction force on an incompletely divided nerve, causing irregular proximal and distal ends. In the majority of patients, nerve roots are still in continuity and can therefore be used for reconstruction of the brachial plexus nerves12). Selection of optimal reconstructive surgery for traumatic BPIs differs among surgeons.
Nerve transfer is a surgical option that intentionally divides a physiologically active nerve and transfers it to a distal, more important but irreparable, paralytic nerve. Nerve transfer can be achieved with several donor nerves, but use of the intercostal nerves remains a popular choice for many surgeons. The motor portion of the intercostal nerve contains 500 to 700 myelinated motor fibers3). Because they are small and contain few motor fibers, three intercostal nerves are usually transferred to restore elbow flexion. The spinal accessory nerve has approximately 1,500 myelinated axons and is often used as a transfer nerve to innervate the suprascapular nerve, or less commonly, the musculocutaneous nerve, for shoulder abduction.
Previous studies have noted that shoulder abduction is best restored by transfer of an accessory nerve to the suprascapular nerve, whereas elbow flexion is best restored using intercostal nerves without grafts7). However, with consideration of the patient’s quality of life, elbow flexion is the priority for brachial plexus reconstruction because it allows for placement of the hand in space. Thus, studies focus on reconstructing the musculocutaneous nerve, proving better outcomes for ICNT with sural nerve grafts on accessory nerves. However, SANT provides better motor recovery, while ICNT provides better pain relief14).
The time interval between trauma and surgery is one of the most important factors in determining surgical outcome2,11,13). Indeed, a substantial number of studies advocate early surgical exploration of the brachial plexus6,10). Furthermore, late-phase nerve reconstructions demonstrated poor outcomes due to nerve degeneration9). Some physicians believe that there is rarely a need for surgery, assuming that most injured nerves that do not regenerate with functional recovery are not amenable to surgical repair. Unfortunately, some patients present for surgery long after the injury occurred, when they are no longer good candidates for a fair outcome.
The population affected by BPIs is heterogeneous, and surgeons must consider various factors when developing an appropriate management plan for each patient. Our study provides a decision framework for considering treatment strategies to manage patients effectively.
CONCLUSION
In our study, we compared different parameters that play an important role in successful musculocutaneous nerve reconstruction for traumatic BPIs. Specifically, combined procedures (ICNT with SANT) produced better results than ICNT alone, and surgery should be performed within 6 months of injury.