INTRODUCTION
Schwannoma is a benign, rarely recurring tumor in the peripheral nerves. Schwann cells, which separate and insulate nerve cells, are glial cells of the peripheral nervous system. In the field of neurosurgery, schwannomas are noted for their specific locations, including the cerebellopontine angle and cranial nerve; however, they are uncommon in the cutaneous nerve. Cutaneous schwannomas develop in the major peripheral nerves and can be located superficially, although they most commonly occur in the subcutaneous layer or even deeper5).
In this report, we present a case of subcutaneous schwannoma of the scalp and discuss its characteristics.
CASE REPORT
The patient was a 45-year-old woman admitted with a palpable scalp mass on the occiput initially noticed 2 years prior. The mass had grown gradually over the last year and has since stabilized at the current size. However, it caused her mild discomfort, particularly while lying down, but no noticeable pain. She reported no head trauma or injection in the scalp. Palpation examination revealed a 1.5 cm-sized round subcutaneous mass, which was soft and exhibited a movable tendency. The margin of the lesion was well circumscribed and contained under the skin, with no signs of skin retraction, openings, or purulent drainage.
Computed tomography (CT) showed a 6 × 12-mm sized soft-tissue density subcutaneous nodule in the right paramedian occipital region. However, no abnormal density was detected in the brain parenchyma and skull (Fig. 1).
Considering all this evidence, we suspected this mass was an epidermal cyst or lipoma. Subsequently, under local anesthesia, the patient elected to undergo surgical excision of the mass. The mass was completely resected, with no postoperative complications. At 3 weeks after the surgery, the surgical wound had completely healed, and the patient’s symptoms had all improved.
Pathology
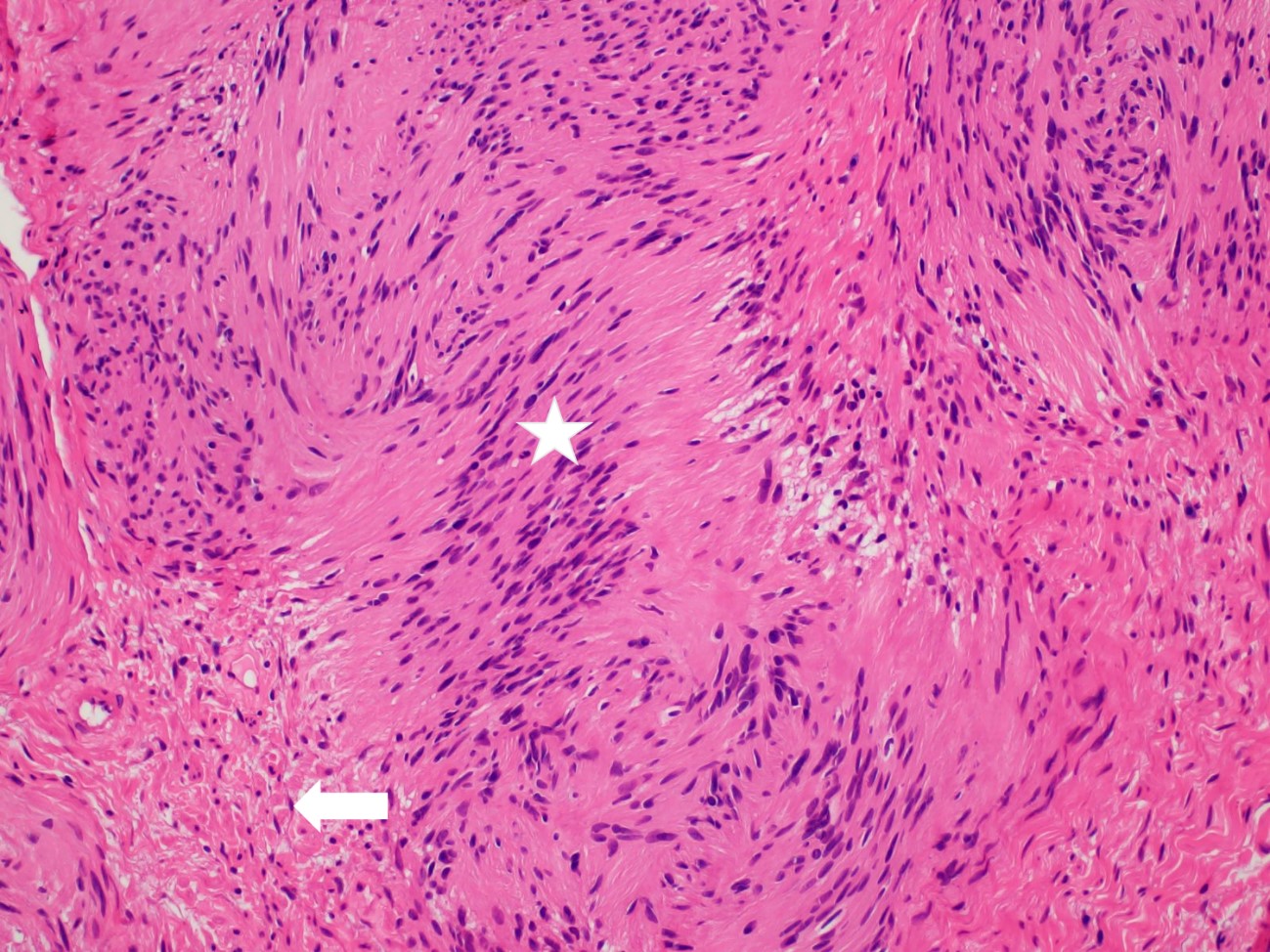
At 1 week after the surgery, a pathological diagnosis was performed. Hematoxylin and eosin staining under a low power field (Original magnification, ×100) revealed that the mass was composed mostly of spindle cells (Fig. 2). Under a high power field (Original magnification, ×400), the staining demonstrated compact spindle cells with characteristic nuclear palisading (Verocay body, Antoni A; asterisk) and loose hypocellular (Antoni B; arrow) areas between the compact cell area, providing reasonable evidence of a schwannoma (Fig. 3).
DISCUSSION
Soft-tissue nodules are common - about two-thirds of soft-tissue tumors are classified into seven diagnostic categories: lipoma and lipoma variants (16%), fibrous histiocytoma (13%), nodular fasciitis (11%), hemangioma (8%), fibromatosis (7%), neurofibroma (5%), and schwannoma (5%)4).
Furthermore, peripheral nerve tumors have several classifications, such as nonneoplastic vs. neoplastic, benign vs. malignant, and sheath vs. non-sheath origins. Schwannoma is considered part of the neoplastic subset due to their growth; otherwise, they are classified as benign with a sheath origin. Compared to neurofibromas, benign schwannomas have a slower rate of progression, lower association with pain, and fewer neurologic symptoms7).
Schwannoma is a neural tumor derived from Schwann cells surrounding the peripheral nerves. The neural sheath comprises three cell types: the fibroblast, Schwann cell, and perineural cell6). Among them, Schwann cells play the important role of developing into a schwannoma. Schwannomas are composed exclusively of Schwann cells located in the nerve sheath, whereas neurofibromas consist of all the different cell types that constitute a nerve2).
Schwannomas are most commonly found in the retroperitoneum (32%), mediastinum (23%), head and neck (18%), and extremities (16%)8). Most schwannoma cases (about 90%) are sporadic, whereas 2% are related to neurofibromatosis type 23). Clinically, these benign tumors are easily mistaken for other lesions, including lipomas and epidermal cysts. Considering that these two lesions account for a large proportion of scalp lesions, the preoperative diagnosis in our case was an epidermal cyst or subcutaneous lipoma. Unfortunately, no clear radiographic imaging was available for differential diagnosis. In our case, the patient underwent non-contrast brain CT scanning, and the lesion showed a high-density round mass similar to that observed in other epidermal/dermal cystic lesions.
Schwannomas are exclusively treated with excision, and they have a good prognosis and low recurrence rate. However, the recurrence rates for completely resected schwannomas of the scalp are unknown because only a few reports are available in the literature. Vestibular schwannomas, which are well known in the neurosurgery field, generally have recurrence rates of 2% to 3% in cases of total resection1). Thus, we believe that the recurrence rates of subcutaneous schwannomas of the scalp may be in this range.
CONCLUSION
Many neurosurgeons consider schwannomas to develop in the cranial nerve; however, our case shows that schwannomas can also present as subcutaneous scalp lesions. Although subcutaneous schwannomas are not different from other soft-tissue masses in terms of treatment, pathological examination should be performed to establish an exact diagnosis.